Complete Health Indicator Report of Blood Pressure: Doctor-diagnosed Hypertension
Definition
The percentage of adults who have ever been told by a doctor, nurse, or other health professionals that they have high blood pressure. This indicator is used to estimate the prevalence of high blood pressure in Utah. Data are from the Utah Behavioral Risk Factor Surveillance System (BRFSS).Numerator
The number of survey respondents who report they have ever been told by a doctor, nurse, or other health professionals that they have high blood pressure.Denominator
The total number of survey respondents (BRFSS survey) excluding those with missing or refused values in the numerator.Data Interpretation Issues
Data are self-reported and subject to respondents' recall and accuracy of reporting. To reduce sampling bias and more accurately represent population data, the BRFSS has changed survey methodology. In 2011, it began conducting surveys by cellular phone in addition to landline phones. It also adopted "iterative proportional fitting" (raking) as its weighting method. More details about these changes can be found at: [https://ibis.health.utah.gov/pdf/opha/resource/brfss/RakingImpact2011.pdf/ Raking Fact Sheet 2011].Why Is This Important?
High blood pressure (hypertension) is an important risk factor for heart disease and stroke. In most cases, it can be effectively managed with medication and lifestyle changes (such as diet, exercise, and abstaining from tobacco use). Treatment works best when high blood pressure is identified early. Because high blood pressure does not produce symptoms, regular screening is recommended. In most cases, high blood pressure is defined as a systolic (upper) number of 140 or greater and a diastolic (lower) number of 90 or greater.Healthy People Objective HDS-5.1:
Reduce the proportion of adults with hypertensionU.S. Target: 26.9 percent
State Target: 22.8 percent
How Are We Doing?
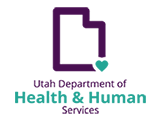
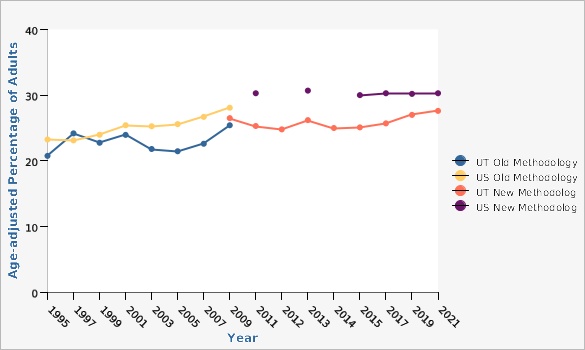
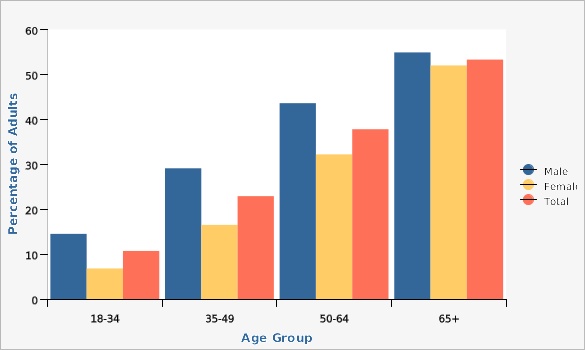
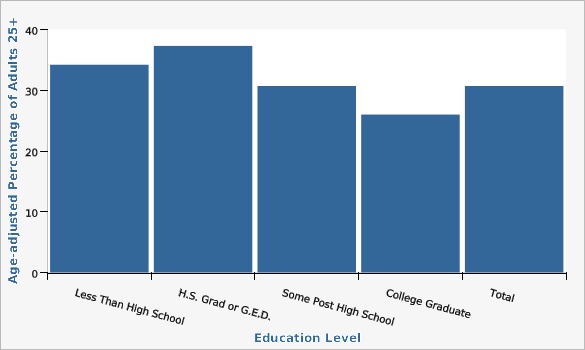
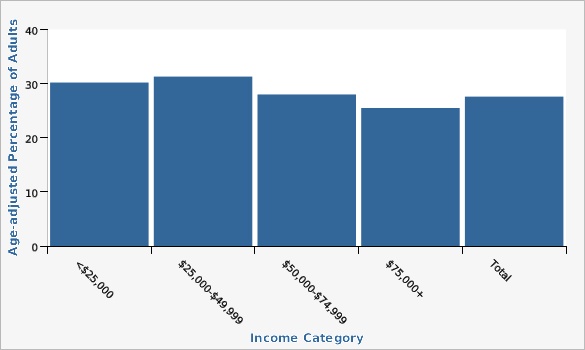
The proportion of Utah adults who reported being told they had high blood pressure has remained relatively stable over the past decade. In 2021, more than one in four (27.6%) Utah adults reported being told they had high blood pressure (age-adjusted rate). The percentage of adults who reported being told they had high blood pressure was much lower for females than males in every age group. The gender differences were less pronounced by age 65 and over. In this age group, the rate of high blood pressure was 54.9% among men and 52.0% for women in 2021 (crude rates). Rates of doctor-diagnosed high blood pressure are somewhat similar among income categories. The rate was 25.5% among those with annual household income above $75,000, and 30.2% among those with household income below $25,000 in 2021 (age-adjusted rate). Doctor-diagnosed high blood pressure varied by educational level. Among college graduates, the rate was 26.0%, lower than the rate for those with less than a high school education (34.2%) in 2021. These rates represent adults aged 25 and over (age-adjusted rates). The rate of doctor-diagnosed high blood pressure was not significantly different between Hispanic (29.0%) and non-Hispanic Utahns (27.6%) in 2021 (age-adjusted rates).How Do We Compare With the U.S.?
In 2021, Utah had a lower age-adjusted high blood pressure prevalence (27.6%) than the U.S. (30.3%).What Is Being Done?
The Healthy Environments Active Living (HEAL) Program was previously known as the Healthy Living through Environment, Policy, and Improved Clinical Care (EPICC) Program. EPICC was created in 2013, consolidating three Utah Department of Health and Human Services (DHHS) programs (the Diabetes Prevention and Control Program, Heart Disease and Stroke Prevention Program, and the Physical Activity, Nutrition, and Obesity Program). The purpose of the consolidation was to ensure a productive, collaborative, and efficient program focused on health outcomes. HEAL aims to reduce the incidence of diabetes, heart disease, and stroke by targeting risk factors including reducing obesity, increasing physical activity, and nutritious food consumption, and improving diabetes and hypertension control. HEAL is part of the Utah Million Hearts Coalition. [https://millionhearts.hhs.gov/index.html Million Hearts 2027] is an initiative co-led by the Centers for Disease Control and Prevention and the Centers for Medicare and Medicaid Services. Million Hearts aimed to reduce the number of heart attacks and strokes in the U.S. by 1 million by 2027. The Utah Million Hearts Coalition has initiated efforts to educate staff in primary care clinics on the proper techniques for measuring high blood pressure.Evidence-based Practices
Health care organizations can improve high blood pressure control among their patient populations. Some strategies that have proven effective and sustainable include: *Maximizing the use of electronic medical records that allow providers to track patient care over time, and incorporate prompts and reminders to improve care. *Integrating team based care that makes full use of the skills of health care team members to identify and treat patients with high blood pressure, provide patient support and follow-up care, and help patients manage their medicines and stick to a blood pressure control plan. *Reinforcing the importance of maintaining behaviors that affect blood pressure, such as eating a healthy, low sodium diet; being physically active; maintaining a healthy weight; and abstaining from smoking.Available Services
The Utah Department of Health and Human Services Healthy Environments Active Living (HEAL) Program works with health care organizations and other partners to improve the accuracy of blood pressure measurement and to improve medication adherence for people with high blood pressure. See the HEAL website for more details: https://heal.health.utah.gov/heart%20health/.Health Program Information
In 2012, DHHS published a statistical report titled The Impact of Heart Disease and Stroke in Utah. This report describes overall patterns in cardiovascular disease and risk factors at the state and national levels and among Utah sub-populations (age group, sex, race, ethnicity, and Utah Small Area). To download the full report, please click [https://heal.health.utah.gov/wp-content/uploads/2021/11/Heart-Disease-and-Stroke-Burden-Report-2012.pdf here]. The Utah Department of Health and Human Services, Healthy Environments Active Living program plays a key role in improving the health of residents in the state of Utah. The program was formed in July 2013 (as EPICC), through a new funding opportunity from the Centers of Disease Control and Prevention (CDC) that allowed for the merging of three previously existing programs: the Heart Disease and Stroke Prevention Program, the Diabetes Prevention and Control Program, and the Physical Activity, Nutrition and Obesity Program, as well as the addition of a school health program. The Healthy Environments Active Living Program (HEAL) was recently restructured as part of this strategic planning process and the new program model focuses on working together with staff and partners to address the social determinants of health while advancing health equity and increasing policy, systems and environment changes. HEAL champions public health initiatives and addresses the challenges of making health awareness and access truly universal and equitable in eight key areas: nutrition, heart health, diabetes, physical activity, schools, child care, community health workers, and worksites. Visit [https://heal.health.utah.gov/ HEAL?s website] for more information.Related Indicators
Relevant Population Characteristics
High blood pressure is one of the most common primary diagnoses in the U.S. (Institute of Medicine, 2010). Risk for developing hypertension increases with age. Oral contraceptives may increase risk of high blood pressure in women, especially if the women are older or obese (American Heart Association Heart Disease and Stroke Statistical Update, 2009).Related Relevant Population Characteristics Indicators:
- Utah Population Characteristics: Age Distribution of the Population
- Utah Population Characteristics: Education Level in the Population
- Utah Population Characteristics: Household Income
- Utah Health Improvement Index (HII)
- Utah Population Characteristics: Poverty, All Persons
- Utah Population Characteristics: Racial and Ethnic Composition of the Population
Health Care System Factors
In 2017, the CDC published a guide titled [https://www.cdc.gov/dhdsp/pubs/guides/best-practices/index.htm "Best Practices for Cardiovascular Disease Prevention Programs"]. This guide outlines 8 effective strategies for lowering high blood pressure and cholesterol levels that can be implemented in health care systems and that involve community-clinical links. These strategies are 1) team-based care, 2) collaborative practice agreements, 3) self-measured blood pressure, 4) self-management and education, 5) reducing medication costs, 6) clinical decision support, 7) community health workers, and 8) medication therapy management.Related Health Care System Factors Indicators:
Risk Factors
Some risk factors for high blood pressure cannot be changed, such as family history and genetics, but some can be reduced through lifestyle changes. These include engaging in regular physical activity, reducing excess weight, tobacco cessation or abstinence, and low-sodium diet. Social and environmental factors such as access to preventive health services, income, and discrimination are also related to the risk of high blood pressure. Certain medications, including over-the-counter medications, can affect blood pressure as well. Individuals are encouraged to discuss their risk factors with a physician and monitor their blood pressure regularly.Related Risk Factors Indicators:
Health Status Outcomes
Uncontrolled high blood pressure is a major risk factor for heart attack, stroke, congestive heart failure, and kidney failure. Controlling high blood pressure through medication and/or lifestyle change can help to reduce the risk.Related Health Status Outcomes Indicators:
Graphical Data Views
The rate of hypertension among Utah adults was significantly lower than the rate for U.S. adults (27.6% vs. 30.3%) in 2021. Data are only collected in odd years.
| BRFSS Utah vs. U.S. | Year | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | ||
|---|---|---|---|---|---|---|
Record Count: 31 | ||||||
| UT Old Methodology | 1995 | 20.8% | 19.0% | 22.6% | ||
| UT Old Methodology | 1997 | 24.2% | 22.2% | 26.3% | ||
| UT Old Methodology | 1999 | 22.8% | 21.0% | 24.6% | ||
| UT Old Methodology | 2001 | 24.0% | 22.3% | 25.7% | ||
| UT Old Methodology | 2003 | 21.8% | 20.3% | 23.4% | ||
| UT Old Methodology | 2005 | 21.5% | 20.3% | 22.7% | ||
| UT Old Methodology | 2007 | 22.6% | 21.4% | 23.8% | ||
| UT Old Methodology | 2009 | 25.4% | 24.5% | 26.4% | ||
| US Old Methodology | 1995 | 23.2% | 22.8% | 23.7% | ||
| US Old Methodology | 1997 | 23.1% | 22.8% | 23.4% | ||
| US Old Methodology | 1999 | 24.0% | 23.6% | 24.3% | ||
| US Old Methodology | 2001 | 25.4% | 25.1% | 25.7% | ||
| US Old Methodology | 2003 | 25.3% | 25.0% | 25.5% | ||
| US Old Methodology | 2005 | 25.6% | 25.4% | 25.9% | ||
| US Old Methodology | 2007 | 26.7% | 26.4% | 26.9% | ||
| US Old Methodology | 2009 | 28.1% | 27.8% | 28.3% | ||
| UT New Methodology | 2009 | 26.5% | 25.6% | 27.5% | ||
| UT New Methodology | 2011 | 25.3% | 24.5% | 26.2% | ||
| UT New Methodology | 2012 | 24.8% | 23.4% | 26.2% | ||
| UT New Methodology | 2013 | 26.2% | 25.3% | 27.0% | ||
| UT New Methodology | 2014 | 25.0% | 23.8% | 26.3% | ||
| UT New Methodology | 2015 | 25.1% | 24.3% | 26.0% | ||
| UT New Methodology | 2017 | 25.7% | 24.8% | 26.7% | ||
| UT New Methodology | 2019 | 27.0% | 26.1% | 28.0% | ||
| UT New Methodology | 2021 | 27.6% | 26.6% | 28.6% | ||
| US New Methodology | 2011 | 30.3% | 30.1% | 30.6% | ||
| US New Methodology | 2013 | 30.7% | 30.5% | 30.9% | ||
| US New Methodology | 2015 | 30.0% | 29.8% | 30.2% | ||
| US New Methodology | 2017 | 30.3% | 30.0% | 30.5% | ||
| US New Methodology | 2019 | 30.2% | 29.9% | 30.4% | ||
| US New Methodology | 2021 | 30.3% | 30.0% | 30.6% | ||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. [[br]] [[br]] Age-adjusted to the 2000 U.S. population. [[br]] [[br]] Note: At the time of this update, the BRFSS U.S. dataset did not include an age variable but did include five age categories up to age 80+ (vs. the typical weighting scheme that includes 85+). Comparisons with both weighting schemes were compared using Utah data, and the difference was about 1/100 of a percentage point. [[br]] [[br]] Beginning in 2011, BRFSS data include both landline and cell phone respondent data along with a new weighting methodology called iterative proportional fitting, or raking. More details about these changes can be found at: [https://ibis.health.utah.gov/pdf/opha/resource/brfss/RakingImpact2011.pdf].Data Sources
- The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)
- Behavioral Risk Factor Surveillance System Survey Data, US Department of Health and Human Services Centers for Disease Control and Prevention (CDC).
In general, high blood pressure prevalence increases with age. Utah males have higher rates of high blood pressure than females in every age category. For adults aged 65 and over, the rates of hypertension for males and females were similar.
| Males vs. Females | Age Group | Percentage of Adults | Lower Limit | Upper Limit | ||
|---|---|---|---|---|---|---|
Record Count: 12 | ||||||
| Male | 18-34 | 14.5% | 12.3% | 17.0% | ||
| Male | 35-49 | 29.1% | 26.2% | 32.1% | ||
| Male | 50-64 | 43.6% | 40.2% | 47.0% | ||
| Male | 65+ | 54.9% | 51.5% | 58.2% | ||
| Female | 18-34 | 6.8% | 5.2% | 8.8% | ||
| Female | 35-49 | 16.5% | 14.2% | 19.1% | ||
| Female | 50-64 | 32.2% | 29.0% | 35.5% | ||
| Female | 65+ | 52.0% | 48.9% | 55.1% | ||
| Total | 18-34 | 10.7% | 9.3% | 12.3% | ||
| Total | 35-49 | 22.9% | 21.0% | 24.9% | ||
| Total | 50-64 | 37.8% | 35.5% | 40.2% | ||
| Total | 65+ | 53.3% | 51.1% | 55.6% | ||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS.Data Source
The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)Rates of hypertension between Hispanic and non-Hispanic adults were similar, although rates were slightly higher for Hispanic adults.
| Hispanic Ethnicity | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 4 | ||||||
| Hispanic/Latino | 29.0% | 25.9% | 32.4% | |||
| Non-Hispanic/Latino | 27.6% | 26.5% | 28.6% | |||
| All Ethnicities | 27.6% | 26.6% | 28.6% | |||
| U.S. | 30.3% | 30.0% | 30.6% | |||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. [[br]] [[br]] Data are age-adjusted to the 2000 U.S. population.Data Source
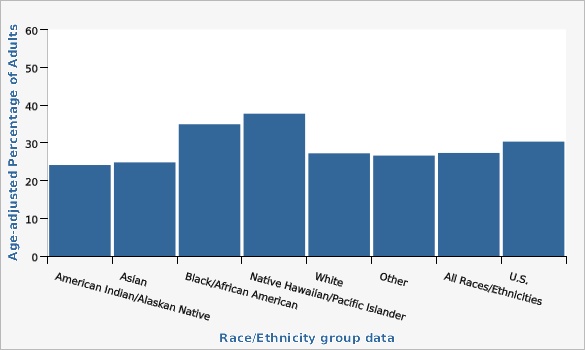
The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)Highest rates of hypertension are seen for adults who are Native Hawaiian/Pacific Islander and adults who are Black/African American.
| Race/Ethnicity group data | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 8 | ||||||
| American Indian/Alaskan Native | 24.1% | 16.7% | 33.4% | |||
| Asian | 24.8% | 17.7% | 33.6% | |||
| Black/African American | 34.9% | 25.7% | 45.4% | |||
| Native Hawaiian/Pacific Islander | 37.7% | 24.2% | 53.4% | |||
| White | 27.2% | 26.2% | 28.3% | |||
| Other | 26.6% | 22.8% | 30.9% | |||
| All Races/Ethnicities | 27.3% | 26.4% | 28.3% | |||
| U.S. | 30.3% | 30.0% | 30.6% | |||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. [[br]] [[br]] Data are age-adjusted to the 2000 U.S. population using 3 groups for age standardization.Data Source
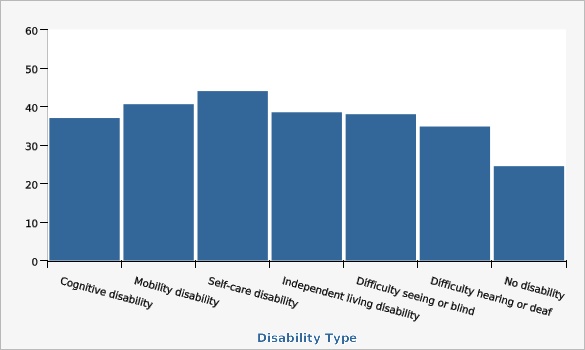
The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)The highest rates of hypertension were seen for adults with self-care disability and mobility disability.
| Disability Type | Lower Limit | Upper Limit | ||||
|---|---|---|---|---|---|---|
Record Count: 7 | ||||||
| Cognitive disability | 37.0% | 33.7% | 40.3% | |||
| Mobility disability | 40.6% | 36.2% | 45.1% | |||
| Self-care disability | 44.0% | 35.6% | 52.7% | |||
| Independent living disability | 38.5% | 34.0% | 43.1% | |||
| Difficulty seeing or blind | 38.0% | 32.1% | 45.5% | |||
| Difficulty hearing or deaf | 34.8% | 29.2% | 40.9% | |||
| No disability | 24.5% | 23.4% | 25.6% | |||
Data Notes
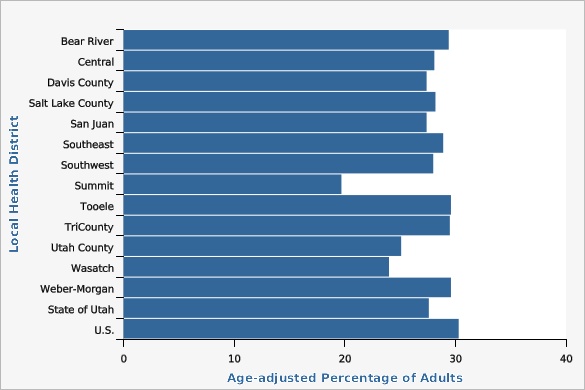
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS.In 2021, Summit County and Wasatch County Local Health Districts had rates of hypertension significantly lower than the state rate.
| Local Health District | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | Note | ||
|---|---|---|---|---|---|---|
Record Count: 15 | ||||||
| Bear River | 29.4% | 25.6% | 33.6% | |||
| Central | 28.1% | 23.9% | 32.7% | |||
| Davis County | 27.4% | 24.2% | 30.8% | |||
| Salt Lake County | 28.2% | 26.5% | 30.0% | |||
| San Juan | 27.4% | 20.4% | 35.6% | |||
| Southeast | 28.9% | 23.3% | 35.2% | |||
| Southwest | 28.0% | 24.1% | 32.4% | |||
| Summit | 19.7% | 15.8% | 24.3% | Lower than the state | ||
| Tooele | 29.6% | 24.9% | 34.8% | |||
| TriCounty | 29.5% | 25.8% | 33.5% | |||
| Utah County | 25.1% | 23.1% | 27.3% | Lower than the State | ||
| Wasatch | 24.0% | 17.7% | 31.6% | |||
| Weber-Morgan | 29.6% | 26.3% | 33.1% | |||
| State of Utah | 27.6% | 26.6% | 28.6% | |||
| U.S. | 30.3% | 30.0% | 30.6% | |||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. [[br]] [[br]] Data are age-adjusted to the 2000 U.S. population.Data Sources
- The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)
- Behavioral Risk Factor Surveillance System Survey Data, US Department of Health and Human Services Centers for Disease Control and Prevention (CDC).
Rates of hypertension generally decrease as education level goes up. Adults who had a college degree or higher had rates of hypertension lower than the state rate.
| Education Level | Age-adjusted Percentage of Adults 25+ | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 5 | ||||||
| Less Than High School | 34.2% | 29.3% | 39.5% | |||
| H.S. Grad or G.E.D. | 37.3% | 34.8% | 39.8% | |||
| Some Post High School | 30.7% | 28.9% | 32.7% | |||
| College Graduate | 26.0% | 24.6% | 27.5% | |||
| Total | 30.7% | 29.6% | 31.8% | |||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. [[br]] [[br]] Adults aged 25 years and older. [[br]] [[br]] Age-adjusted to 2000 U.S. standard population.Data Source
The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)Adults in households with an annual income between $25,000 and $49,999 had a higher hypertension rate than the state. Adults with an income of $75,000 or more had the lowest hypertension rate in the state.
| Income Category | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 5 | ||||||
| <$25,000 | 30.2% | 26.6% | 34.0% | |||
| $25,000-$49,999 | 31.3% | 28.7% | 34.1% | |||
| $50,000-$74,999 | 28.0% | 25.4% | 30.6% | |||
| $75,000+ | 25.5% | 24.0% | 27.0% | |||
| Total | 27.6% | 26.6% | 28.6% | |||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. [[br]] [[br]] Age-adjusted to 2000 U.S. standard population.Data Source
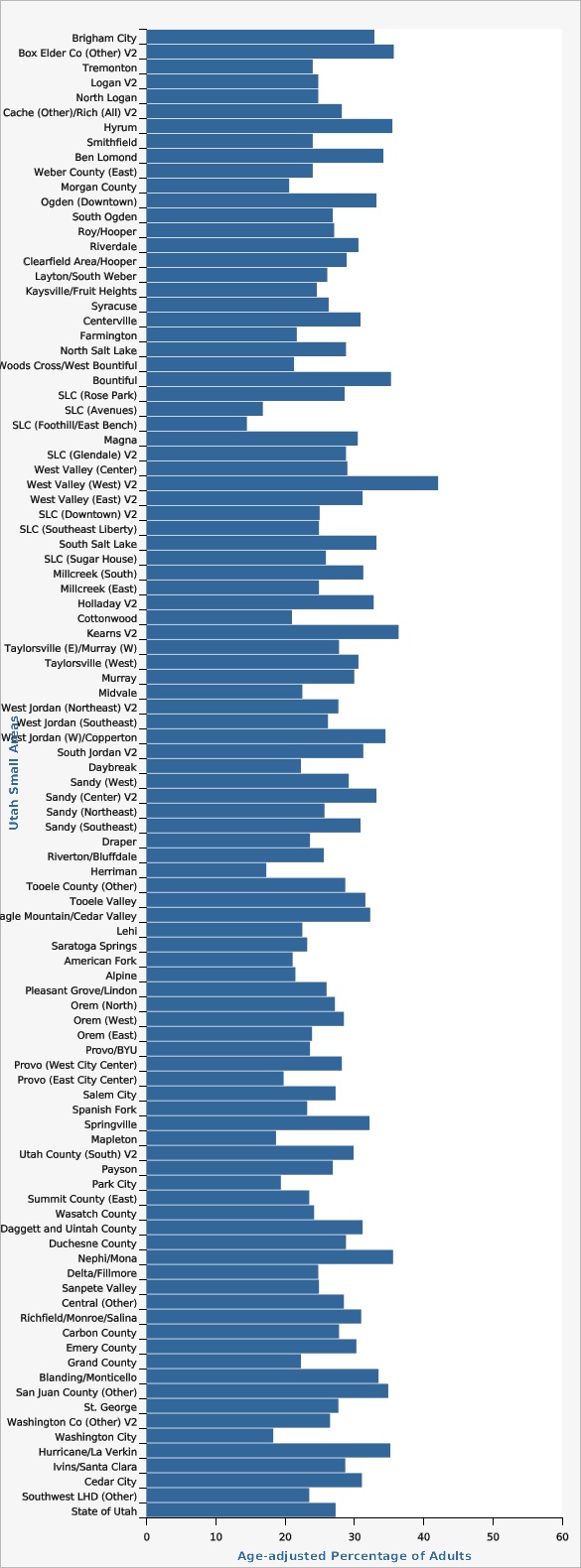
The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)The following Utah Small Areas had higher rates of hypertension than the state: Ben Lomond, Bountiful, West Valley (West), Kearns, West Jordan (West)/Copperton, Tooele Valley, and Daggett and Uintah County. Small areas with rates of hypertension that were significantly lower than the state were: Salt Lake City (Avenues), Salt Lake City (Foothill/East Bench), Cottonwood, Herriman, American Fork, Park City, and Washington City.
| Utah Small Areas | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | Note | ||
|---|---|---|---|---|---|---|
Record Count: 100 | ||||||
| Brigham City | 32.9% | 25.3% | 41.5% | |||
| Box Elder Co (Other) V2 | 35.7% | 25.2% | 47.7% | |||
| Tremonton | 24.0% | 17.2% | 32.5% | |||
| Logan V2 | 24.8% | 20.1% | 30.2% | |||
| North Logan | 24.8% | 18.2% | 32.8% | |||
| Cache (Other)/Rich (All) V2 | 28.2% | 21.9% | 35.5% | |||
| Hyrum | 35.5% | 24.6% | 48.2% | |||
| Smithfield | 24.0% | 17.1% | 32.5% | |||
| Ben Lomond | 34.2% | 29.4% | 39.3% | Higher than the state | ||
| Weber County (East) | 24.0% | 18.7% | 30.2% | |||
| Morgan County | 20.6% | 13.5% | 30.1% | |||
| Ogden (Downtown) | 33.2% | 27.0% | 39.9% | |||
| South Ogden | 26.9% | 21.4% | 33.2% | |||
| Roy/Hooper | 27.1% | 22.0% | 33.0% | |||
| Riverdale | 30.6% | 23.0% | 39.5% | |||
| Clearfield Area/Hooper | 28.9% | 24.2% | 34.2% | |||
| Layton/South Weber | 26.1% | 22.1% | 30.4% | |||
| Kaysville/Fruit Heights | 24.6% | 19.2% | 30.9% | |||
| Syracuse | 26.3% | 20.0% | 33.8% | |||
| Centerville | 30.9% | 21.6% | 42.1% | |||
| Farmington | 21.7% | 15.2% | 30.0% | |||
| North Salt Lake | 28.8% | 19.5% | 40.3% | |||
| Woods Cross/West Bountiful | 21.3% | 13.3% | 32.4% | |||
| Bountiful | 35.3% | 29.1% | 42.1% | Higher than the state | ||
| SLC (Rose Park) | 28.6% | 21.9% | 36.4% | |||
| SLC (Avenues) | 16.8% | 10.6% | 25.5% | Lower than the state | ||
| SLC (Foothill/East Bench) | 14.5% | 9.7% | 21.2% | |||
| Magna | 30.5% | 23.8% | 38.1% | Lower than the state | ||
| SLC (Glendale) V2 | 28.8% | 19.6% | 40.2% | |||
| West Valley (Center) | 29.0% | 23.3% | 35.4% | |||
| West Valley (West) V2 | 42.1% | 32.9% | 51.9% | Higher than the state | ||
| West Valley (East) V2 | 31.2% | 24.9% | 38.3% | |||
| SLC (Downtown) V2 | 25.0% | 18.7% | 32.7% | |||
| SLC (Southeast Liberty) | 24.9% | 17.1% | 34.8% | |||
| South Salt Lake | 33.2% | 25.9% | 41.4% | |||
| SLC (Sugar House) | 25.9% | 19.9% | 33.0% | |||
| Millcreek (South) | 31.3% | 22.9% | 41.0% | |||
| Millcreek (East) | 24.9% | 18.0% | 33.2% | |||
| Holladay V2 | 32.8% | 24.9% | 41.7% | |||
| Cottonwood | 21.0% | 16.4% | 26.4% | Lower than the state | ||
| Kearns V2 | 36.4% | 29.5% | 43.9% | Higher than the state | ||
| Taylorsville (E)/Murray (W) | 27.8% | 22.7% | 33.5% | |||
| Taylorsville (West) | 30.6% | 24.6% | 37.4% | |||
| Murray | 30.0% | 23.2% | 37.9% | |||
| Midvale | 22.5% | 16.4% | 30.0% | |||
| West Jordan (Northeast) V2 | 27.7% | 21.5% | 35.0% | |||
| West Jordan (Southeast) | 26.2% | 20.8% | 32.5% | |||
| West Jordan (W)/Copperton | 34.5% | 27.4% | 42.3% | Higher than the state | ||
| South Jordan V2 | 31.3% | 25.1% | 38.3% | |||
| Daybreak | 22.3% | 16.2% | 29.8% | |||
| Sandy (West) | 29.2% | 22.2% | 37.4% | |||
| Sandy (Center) V2 | 33.2% | 26.0% | 41.4% | |||
| Sandy (Northeast) | 25.7% | 19.3% | 33.3% | |||
| Sandy (Southeast) | 30.9% | 23.4% | 39.6% | |||
| Draper | 23.6% | 17.8% | 30.7% | |||
| Riverton/Bluffdale | 25.6% | 20.7% | 31.3% | |||
| Herriman | 17.3% | 13.0% | 22.6% | Lower than the state | ||
| Tooele County (Other) | 28.7% | 22.1% | 36.2% | |||
| Tooele Valley | 31.6% | 27.7% | 35.8% | Higher than the state | ||
| Eagle Mountain/Cedar Valley | 32.3% | 26.6% | 38.5% | |||
| Lehi | 22.5% | 18.1% | 27.5% | |||
| Saratoga Springs | 23.2% | 16.3% | 31.9% | |||
| American Fork | 21.1% | 16.8% | 26.3% | Lower than the state | ||
| Alpine | 21.5% | 13.4% | 32.6% | |||
| Pleasant Grove/Lindon | 26.0% | 21.7% | 30.9% | |||
| Orem (North) | 27.2% | 21.1% | 34.2% | |||
| Orem (West) | 28.5% | 22.3% | 35.6% | |||
| Orem (East) | 23.9% | 17.4% | 31.8% | |||
| Provo/BYU | 23.6% | 17.4% | 31.2% | |||
| Provo (West City Center) | 28.2% | 22.6% | 34.6% | |||
| Provo (East City Center) | 19.8% | 13.0% | 29.0% | |||
| Salem City | 27.3% | 17.0% | 40.8% | |||
| Spanish Fork | 23.2% | 18.5% | 28.8% | |||
| Springville | 32.2% | 25.5% | 39.8% | |||
| Mapleton | 18.7% | 11.8% | 28.4% | |||
| Utah County (South) V2 | 29.9% | 21.8% | 39.5% | |||
| Payson | 26.9% | 20.8% | 34.2% | |||
| Park City | 19.4% | 13.7% | 26.6% | Lower than the state | ||
| Summit County (East) | 23.5% | 17.9% | 30.3% | |||
| Wasatch County | 24.2% | 19.6% | 29.5% | |||
| Daggett and Uintah County | 31.2% | 27.5% | 35.2% | Higher than the state | ||
| Duchesne County | 28.8% | 23.3% | 34.9% | |||
| Nephi/Mona | 35.6% | 25.6% | 47.1% | |||
| Delta/Fillmore | 24.8% | 17.7% | 33.4% | |||
| Sanpete Valley | 24.9% | 19.2% | 31.5% | |||
| Central (Other) | 28.5% | 23.4% | 34.2% | |||
| Richfield/Monroe/Salina | 31.0% | 24.9% | 37.9% | |||
| Carbon County | 27.8% | 23.2% | 32.9% | |||
| Emery County | 30.3% | 22.2% | 39.8% | |||
| Grand County | 22.3% | 16.0% | 30.2% | |||
| Blanding/Monticello | 33.5% | 24.9% | 43.2% | |||
| San Juan County (Other) | 34.9% | 24.5% | 46.9% | |||
| St. George | 27.7% | 23.6% | 32.2% | |||
| Washington Co (Other) V2 | 26.5% | 17.3% | 38.3% | |||
| Washington City | 18.3% | 13.1% | 24.9% | Lower than the state | ||
| Hurricane/La Verkin | 35.2% | 27.3% | 44.1% | |||
| Ivins/Santa Clara | 28.7% | 18.0% | 42.5% | |||
| Cedar City | 31.1% | 25.0% | 38.1% | |||
| Southwest LHD (Other) | 23.5% | 17.4% | 30.8% | |||
| State of Utah | 27.3% | 26.6% | 28.0% | |||
Data Notes
Doctor-diagnosed hypertension is based on the answer to the question: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" Response options are: "Yes", "No", "Yes but females told only during pregnancy, and "Told borderline high or pre-hypertensive." Women who report having hypertension only during pregnancy and individuals who are told they are borderline high are considered as having answered "No." In 2016, Utah BRFSS modified its methodology for age adjustment to increase the precision of the estimate. Data in IBIS charts have been updated back to 2011 forward to reflect this change. With this change, age adjustment for Utah is more consistent with both the U.S. and other states using IBIS. [[br]] [[br]] Age-adjusted to U.S. 2000 standard population. [[br]] Data are for combined years 2019 and 2021. [[br]] A description of the Utah Small Areas may be found on the Methodology and Guidelines page: [https://ibis.health.utah.gov/resource/Guidelines.html].Data Source
The Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS)References and Community Resources
'''Impact of Heart Disease and Stroke in Utah''' In 2012, the Utah Heart Disease and Stroke Prevention Program published a statistical report titled the Impact of Heart Disease and Stroke in Utah. This report describes overall patterns in cardiovascular disease and risk factors at the state and national levels and among Utah subpopulations (age group, sex, race, ethnicity, and Utah Small Area). '''Million Hearts Initiative''' Heart disease and stroke are the first and fifth leading causes of death in the United States (CDC 2022). Heart disease is responsible for 1 of every 3 deaths in the country. Million Hearts is a national initiative that has set an ambitious goal to prevent 1 million heart attacks and strokes within 5 years (by 2027). Million Hearts aims to prevent heart disease and stroke by: *Improving access to effective care *Improving the quality of care for the ABCS (appropriate aspirin prescription, blood pressure control, cholesterol control, and smoking cessation) *Focusing clinical attention on the prevention of heart attack and stroke *Activating the public to lead a heart-healthy lifestyle *Improving the prescription and adherence to appropriate medications for the ABCS See what you can do to be part of the solution. Visit https://millionhearts.hhs.gov/ for more information. CDC's Blood Pressure website: http://www.cdc.gov/bloodpressure/ American Heart Association http://www.heart.org/HEARTORG/More Resources and Links
Evidence-based community health improvement ideas and interventions may be found at the following sites:- Centers for Disease Control and Prevention (CDC) WONDER Database, a system for disseminating public health data and information.
- United States Census Bureau data dashboard.
- Utah healthy Places Index, evidence-based and peer-reviewed tool, supports efforts to prioritize equitable community investments, develop critical programs and policies across the state, and much more.
- County Health Rankings
- Kaiser Family Foundation's StateHealthFacts.org
- Medical literature can be queried at PubMed library.
Page Content Updated On 11/25/2022,
Published on 11/30/2022