Complete Health Indicator Report of Lynch Syndrome (Cancer)
Definition
The rate of colorectal or endometrial cancer incidence in Utah or U.S. per 100,000 persons or females (respectively).Numerator
The number of colorectal or endometrial cancer cases among Utah or U.S. for a specified time period.Denominator
The overall (colorectal) and female (endometrial) population of Utah or U.S. for a specified time period.Why Is This Important?
Hereditary cancer syndromes are genetic predispositions for certain types of cancer that can be passed down through generations. Lynch Syndrome is caused by inherited mutations in genes that prevent them from working properly to protect you from certain cancers including colorectal, endometrial (uterine), and other cancers.^1^ While hereditary cancers only account for about 10% of all cancers, people with a family history of hereditary cancers are at higher risk for getting cancer more than once in their lifetimes, more likely to get cancer at a young age, and are more likely to be diagnosed when the cancer is at a later, more advanced stage.^2^ [[br]] [[br]] ---- 1. Centers for Disease Control and Prevention. (2020, Jan 15). Lynch Syndrome. [[https://www.cdc.gov/genomics/disease/colorectal_cancer/lynch.htm]] [[br]] 2. Centers for Disease Control and Prevention. (2020, Aug 03). Cancer Genomics Program. [[https://www.cdc.gov/cancer/dcpc/about/genomics/index.htm]]Healthy People Objective G-2:
(Developmental) Increase the proportion of persons with newly diagnosed colorectal cancer who receive genetic testing to identify Lynch syndrome (or familial colorectal cancer syndromes)U.S. Target: Developmental
Other Objectives
'''Utah Cancer Action Network Targets for Change:''' [[br]] Reduce the rate of colorectal cancer diagnosed at an advanced (regional or distant) stage among adults ages 50 to 74. [[br]] '''Utah 2020 Target:''' 32 per 100,000 populationHow Are We Doing?
The age-adjusted colorectal cancer under 50 years old incidence rate in Utah has increased over the years. Additionally, the age-adjusted endometrial cancer under 50 incidence rate has increased over the years and has even spiked in certain years.How Do We Compare With the U.S.?
Throughout the years, the Utah colorectal cancer incidence rate has been consistently lower than the U.S. colorectal cancer rate. In comparison, the Utah endometrial cancer incidence rate has been intermittently higher than the U.S. endometrial cancer rate.What Is Being Done?
The Utah Cancer Genomics Program (UCGP) collaborates with community organizations and health systems to provide public/provider education, improve referral processes, and improve access to genetic counseling and testing. These organizations reach many populations throughout the state and provide a variety of services. The UCGP holds an annual Request for Proposals (RFP) competitive application process and awards funding to innovative projects that have the potential to drive Policy, Systems, and Environmental change in public awareness of Family Health History and referral to and uptake of appropriate genetic services. This mini-grant enables strong partnerships between the UCGP and health systems, clinics, and community-based organizations and expands the program's reach into the community. In addition, the UCGP participates in the Utah Cancer Action Network (UCAN), a statewide partnership whose goal is to reduce the burden of cancer. The mission of UCAN is to lower cancer incidence and mortality in Utah through collaborative efforts directed toward cancer prevention and control. As a result of this planning process, objectives and strategies have been developed by community partners regarding the early detection of cervical, breast, and colorectal cancers, and separate cancer genomics collaboration opportunities are also available.Evidence-based Practices
Persons with a family history of colorectal cancer should consult with their health care provider to determine their risk. High-risk individuals should work with their provider to have earlier and more frequent colonoscopies. Individuals diagnosed with Lynch Syndrome should also work with health care professionals to determine family members to contact and consider Cascade Screening.Available Services
Coverage of colorectal cancer screening tests such as colonoscopies and other colorectal cancer screening tests is required by the Affordable Care Act (ACA). However, genetic testing for Lynch Syndrome is not covered by the ACA. Some private insurers may cover testing, but it is likely that deductibles, copays, and cost-sharing will apply. You can find out your insurance plan's benefits and covered services by contacting your health insurance company or your employer's human resources department. There are other screening procedures for Lynch Syndrome, including Universal Screening. Universal Screening involves tumor testing every newly diagnosed colorectal or endometrial cancer case for genes associated with Lynch Syndrome. This tumor testing looks for characteristics of tumor tissue that indicate a mutation in one of the genes associated with Lynch Syndrome by using microsatellite instability (MSI) and immunohistochemistry (IHC). If the tumor testing comes back positive then the person is referred on to genetic testing and germline testing. The aim of this is to identify more persons with Lynch Syndrome and thus get those persons into the proper screening schedule in order to reduce morbidity and mortality from Lynch Syndrome-related cancers. While genetic testing is not always covered by health insurance, Universal Screening may be more accessible if your insurance covers cancer biopsies. Check with your health plan to determine if diagnostic tests after cancer screening are covered.Health Program Information
In 2014 the Utah Department of Health received funding from the CDC to implement a program focused on addressing the cancer burden associated with hereditary cancer syndromes. The UCGP continues to receive funding from the CDC for surveillance, education, improving access to and referrals to genetic services, and bolstering partnerships with healthcare organizations, non-profit organizations, and other community organizations.Related Indicators
Relevant Population Characteristics
Persons without health insurance are less likely to undergo cancer screenings, which can delay access to necessary services including cancer treatment and genetic counseling and testing. Additionally, people are more likely to receive screening as their level of education increases. Screening is vital in diagnosing potential hereditary cancers, so it is important to examine the potential barriers to screening for Utahns.Related Relevant Population Characteristics Indicators:
Health Care System Factors
According to data collected by the Utah Behavioral Risk Factor Surveillance System (BRFSS) screening rates for all Utahns remain lower than previous years and lower than the target rates for all Utahns remain lower than previous years and lower than the target rates set by the Utah State Cancer Plan (80%). Additionally, use of colonoscopies is lower among persons without health insurance compared to persons with health insurance. Coverage of colorectal cancer screening tests such as colonoscopies and other colorectal cancer screening tests is required by the Affordable Care Act (ACA). Despite colorectal cancer screenings being available to all, rates can be improved for all regardless of insurance status. Screening is vital in diagnosing potential hereditary cancers, so it is important to examine the potential barriers to screening for Utahns.Related Health Care System Factors Indicators:
Related Health Status Outcomes Indicators:
Graphical Data Views
Colorectal Cancer Incidence Under Age 50 by Year, Utah and U.S., 1999-2018
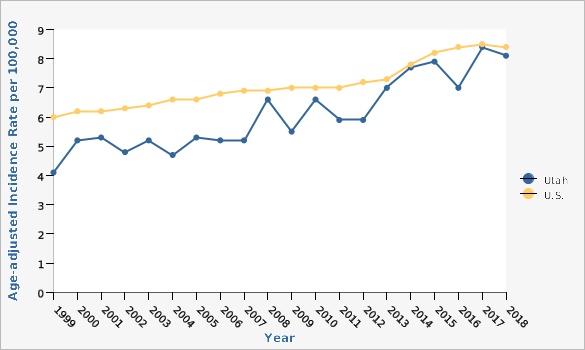
| Utah vs. U.S. | Year | Age-adjusted Incidence Rate per 100,000 | ||||
|---|---|---|---|---|---|---|
Record Count: 40 | ||||||
| Utah | 1999 | 4.1 | ||||
| Utah | 2000 | 5.2 | ||||
| Utah | 2001 | 5.3 | ||||
| Utah | 2002 | 4.8 | ||||
| Utah | 2003 | 5.2 | ||||
| Utah | 2004 | 4.7 | ||||
| Utah | 2005 | 5.3 | ||||
| Utah | 2006 | 5.2 | ||||
| Utah | 2007 | 5.2 | ||||
| Utah | 2008 | 6.6 | ||||
| Utah | 2009 | 5.5 | ||||
| Utah | 2010 | 6.6 | ||||
| Utah | 2011 | 5.9 | ||||
| Utah | 2012 | 5.9 | ||||
| Utah | 2013 | 7.0 | ||||
| Utah | 2014 | 7.7 | ||||
| Utah | 2015 | 7.9 | ||||
| Utah | 2016 | 7.0 | ||||
| Utah | 2017 | 8.4 | ||||
| Utah | 2018 | 8.1 | ||||
| U.S. | 1999 | 6.0 | ||||
| U.S. | 2000 | 6.2 | ||||
| U.S. | 2001 | 6.2 | ||||
| U.S. | 2002 | 6.3 | ||||
| U.S. | 2003 | 6.4 | ||||
| U.S. | 2004 | 6.6 | ||||
| U.S. | 2005 | 6.6 | ||||
| U.S. | 2006 | 6.8 | ||||
| U.S. | 2007 | 6.9 | ||||
| U.S. | 2008 | 6.9 | ||||
| U.S. | 2009 | 7.0 | ||||
| U.S. | 2010 | 7.0 | ||||
| U.S. | 2011 | 7.0 | ||||
| U.S. | 2012 | 7.2 | ||||
| U.S. | 2013 | 7.3 | ||||
| U.S. | 2014 | 7.8 | ||||
| U.S. | 2015 | 8.2 | ||||
| U.S. | 2016 | 8.4 | ||||
| U.S. | 2017 | 8.5 | ||||
| U.S. | 2018 | 8.4 | ||||
Data Notes
Age-adjusted to the U.S. 2000 standard populationData Sources
- Population Estimates: National Center for Health Statistics (NCHS) through a collaborative agreement with the U.S. Census Bureau, IBIS Version 2020
- Cancer data provided by the Utah Cancer Registry, supported by the National Cancer Institute (HHSN261201800016I), the U.S. Center for Disease Control and Prevention (NU58DP0063200), the University of Utah, and Huntsman Cancer Foundation
- U.S. Cancer Statistics: WONDER Online Database. United States Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. Accessed at [http://wonder.cdc.gov/cancer.html]
Endometrial Cancer Incidence Under Age 50 by Year, Utah and U.S., 1999-2018
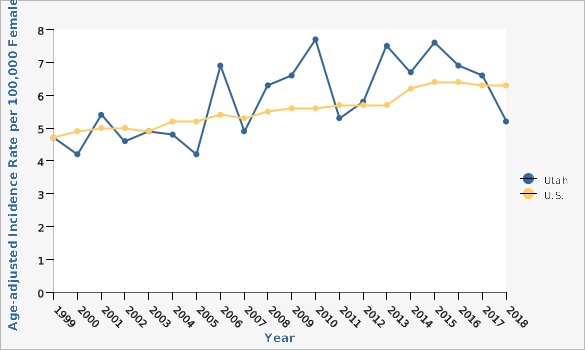
| Utah vs. U.S. | Year | Age-adjusted Incidence Rate per 100,000 Females | ||||
|---|---|---|---|---|---|---|
Record Count: 40 | ||||||
| Utah | 1999 | 4.7 | ||||
| Utah | 2000 | 4.2 | ||||
| Utah | 2001 | 5.4 | ||||
| Utah | 2002 | 4.6 | ||||
| Utah | 2003 | 4.9 | ||||
| Utah | 2004 | 4.8 | ||||
| Utah | 2005 | 4.2 | ||||
| Utah | 2006 | 6.9 | ||||
| Utah | 2007 | 4.9 | ||||
| Utah | 2008 | 6.3 | ||||
| Utah | 2009 | 6.6 | ||||
| Utah | 2010 | 7.7 | ||||
| Utah | 2011 | 5.3 | ||||
| Utah | 2012 | 5.8 | ||||
| Utah | 2013 | 7.5 | ||||
| Utah | 2014 | 6.7 | ||||
| Utah | 2015 | 7.6 | ||||
| Utah | 2016 | 6.9 | ||||
| Utah | 2017 | 6.6 | ||||
| Utah | 2018 | 5.2 | ||||
| U.S. | 1999 | 4.7 | ||||
| U.S. | 2000 | 4.9 | ||||
| U.S. | 2001 | 5.0 | ||||
| U.S. | 2002 | 5.0 | ||||
| U.S. | 2003 | 4.9 | ||||
| U.S. | 2004 | 5.2 | ||||
| U.S. | 2005 | 5.2 | ||||
| U.S. | 2006 | 5.4 | ||||
| U.S. | 2007 | 5.3 | ||||
| U.S. | 2008 | 5.5 | ||||
| U.S. | 2009 | 5.6 | ||||
| U.S. | 2010 | 5.6 | ||||
| U.S. | 2011 | 5.7 | ||||
| U.S. | 2012 | 5.7 | ||||
| U.S. | 2013 | 5.7 | ||||
| U.S. | 2014 | 6.2 | ||||
| U.S. | 2015 | 6.4 | ||||
| U.S. | 2016 | 6.4 | ||||
| U.S. | 2017 | 6.3 | ||||
| U.S. | 2018 | 6.3 | ||||
Data Notes
Age-adjusted to the U.S. 2000 standard populationData Sources
- Population Estimates: National Center for Health Statistics (NCHS) through a collaborative agreement with the U.S. Census Bureau, IBIS Version 2020
- Cancer data provided by the Utah Cancer Registry, supported by the National Cancer Institute (HHSN261201800016I), the U.S. Center for Disease Control and Prevention (NU58DP0063200), the University of Utah, and Huntsman Cancer Foundation
- U.S. Cancer Statistics: WONDER Online Database. United States Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. Accessed at [http://wonder.cdc.gov/cancer.html]
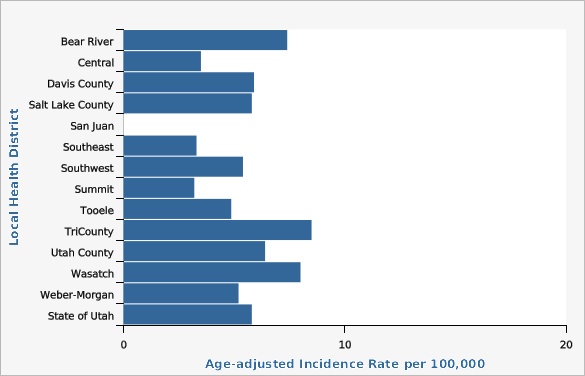
| Local Health District | Age-adjusted Incidence Rate per 100,000 | Lower Limit | Upper Limit | Note | ||
|---|---|---|---|---|---|---|
Record Count: 14 | ||||||
| Bear River | 7.4 | 5.2 | 9.6 | |||
| Central | 3.5 | 1.6 | 6.4 | * | ||
| Davis County | 5.9 | 4.7 | 7.3 | |||
| Salt Lake County | 5.8 | 5.2 | 6.6 | |||
| San Juan | ** | 0.0 | 10.6 | ** | ||
| Southeast | 3.3 | 1.1 | 7.7 | * | ||
| Southwest | 5.4 | 3.9 | 7.3 | |||
| Summit | 3.2 | 1.2 | 7.1 | * | ||
| Tooele | 4.9 | 2.7 | 8.1 | |||
| TriCounty | 8.5 | 5.1 | 13.4 | |||
| Utah County | 6.4 | 5.4 | 7.6 | |||
| Wasatch | 8.0 | 4.0 | 14.4 | |||
| Weber-Morgan | 5.2 | 3.9 | 6.7 | |||
| State of Utah | 5.8 | 5.4 | 6.3 | |||
Data Notes
Age-adjusted to the U.S. 2000 standard population [[br]] Note: Prior to 2015 San Juan County was part of the Southeast Local Health District. In 2015 the San Juan Local Health District was formed. Data reported are for all years using the current boundaries. [[br]] [[br]] *Use caution in interpreting, the estimate has a relative standard error greater than 30% and does not meet UDOH standards for reliability. For more information, please go to [http://ibis.health.utah.gov/pdf/resource/DataSuppression.pdf]. [[br]]**The estimate has been suppressed because the observed number of events is very small and not appropriate for publication.Data Source
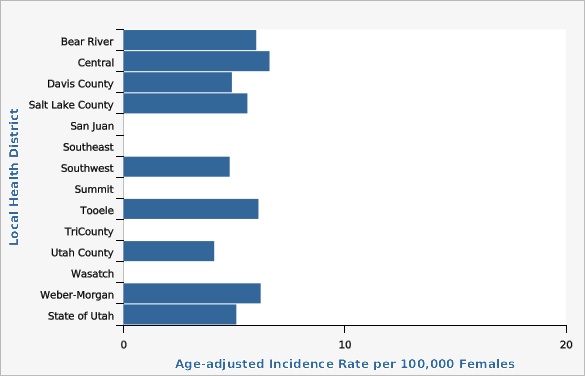
Cancer data provided by the Utah Cancer Registry, supported by the National Cancer Institute (HHSN261201800016I), the U.S. Center for Disease Control and Prevention (NU58DP0063200), the University of Utah, and Huntsman Cancer Foundation| Local Health District | Age-adjusted Incidence Rate per 100,000 Females | Lower Limit | Upper Limit | Note | ||
|---|---|---|---|---|---|---|
Record Count: 14 | ||||||
| Bear River | 6.0 | 3.5 | 9.4 | |||
| Central | 6.6 | 3.0 | 12.5 | * | ||
| Davis County | 4.9 | 3.4 | 6.8 | |||
| Salt Lake County | 5.6 | 4.7 | 6.6 | |||
| San Juan | ** | ** | ||||
| Southeast | ** | 0.3 | 9.5 | ** | ||
| Southwest | 4.8 | 2.9 | 7.5 | |||
| Summit | ** | 0.3 | 8.6 | ** | ||
| Tooele | 6.1 | 2.8 | 11.7 | * | ||
| TriCounty | ** | 0.2 | 6.3 | ** | ||
| Utah County | 4.1 | 2.9 | 5.6 | |||
| Wasatch | ** | 0.4 | 11.7 | ** | ||
| Weber-Morgan | 6.2 | 4.3 | 8.8 | |||
| State of Utah | 5.1 | 4.5 | 5.7 | |||
Data Notes
Age-adjusted to the U.S. 2000 standard population [[br]] Note: Prior to 2015 San Juan County was part of the Southeast Local Health District. In 2015 the San Juan Local Health District was formed. Data reported are for all years using the current boundaries. [[br]] [[br]] *Use caution in interpreting, the estimate has a relative standard error greater than 30% and does not meet UDOH standards for reliability. For more information, please go to [http://ibis.health.utah.gov/pdf/resource/DataSuppression.pdf]. [[br]]**The estimate has been suppressed because the observed number of events is very small and not appropriate for publication.Data Source
Cancer data provided by the Utah Cancer Registry, supported by the National Cancer Institute (HHSN261201800016I), the U.S. Center for Disease Control and Prevention (NU58DP0063200), the University of Utah, and Huntsman Cancer FoundationData Notes
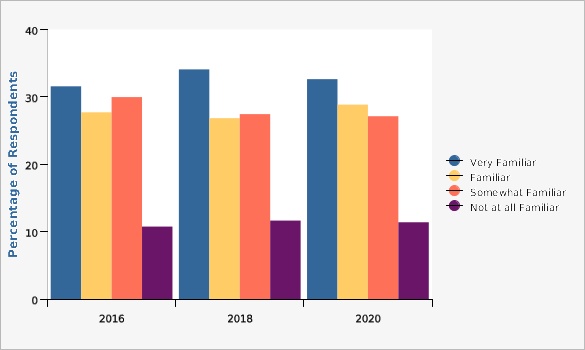
How familiar are you with your family history of cancer among blood relatives including your parents, grandparents, siblings, aunts, uncles, and children?Data Source
Utah Data: Behavioral Risk Factor Surveillance System, Office of Public Health Assessment, Utah Department of HealthData Notes
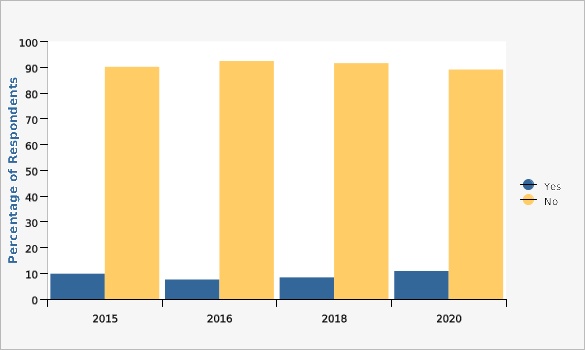
Has a doctor, nurse, or other healthcare provider ever talked to you about genetic testing if you or your family are at increased risk for developing breast, ovarian, colorectal, or uterine cancer?Data Source
Utah Data: Behavioral Risk Factor Surveillance System, Office of Public Health Assessment, Utah Department of HealthData Notes
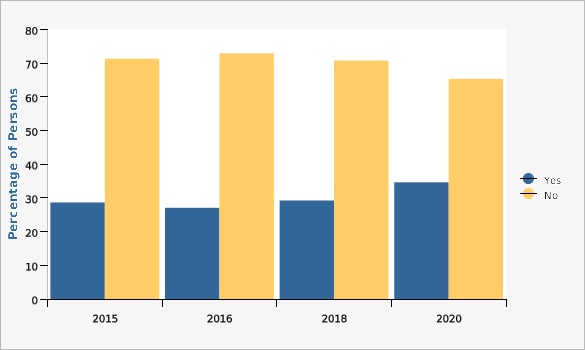
Have you ever had a genetic test to determine if you or your family is at increased risk of developing cancer? [[br]] [[br]]*Question only asked to those who answered "yes", "don't know", or "refused" to previous question, 'Has a doctor, nurse, or other healthcare provider ever talked to you about genetic testing if you or your family are at increased risk for developing breast, ovarian, colorectal, or uterine cancer?'Data Source
Utah Data: Behavioral Risk Factor Surveillance System, Office of Public Health Assessment, Utah Department of HealthData Notes
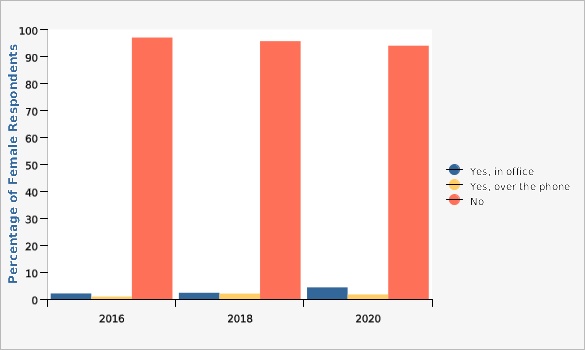
Have you ever met with a genetic counselor to discuss your risk of breast and ovarian cancer?Data Source
Utah Data: Behavioral Risk Factor Surveillance System, Office of Public Health Assessment, Utah Department of HealthReferences and Community Resources
For more information about Lynch Syndrome and financial assistance opportunities, please visit: *The University of Utah Huntsman Cancer Institute's resource page @ [https://hci-portal.hci.utah.edu/sites/lynchsyndrome_patientinfo/_layouts/15/start.aspx#/] *The University of Utah Huntsman Cancer Institute has a Financial Assistance Policy in place that may allow partial or full reduction of your bill based on household income. Financial Advocates are available to answer any questions at 1(800) 862-4937 *Intermountain Healthcare offers a Financial Assistance Program to individuals and families earning up to 500% of the federal poverty level. Call 1(866) 415-6556 *Steward provides discounts and payment plans to patients who quality. Call (888) 554-0228More Resources and Links
Evidence-based community health improvement ideas and interventions may be found at the following sites:- Centers for Disease Control and Prevention (CDC) WONDER Database, a system for disseminating public health data and information.
- United States Census Bureau data dashboard.
- Utah healthy Places Index, evidence-based and peer-reviewed tool, supports efforts to prioritize equitable community investments, develop critical programs and policies across the state, and much more.
- County Health Rankings
- Kaiser Family Foundation's StateHealthFacts.org
- Medical literature can be queried at PubMed library.
Page Content Updated On 02/22/2022,
Published on 03/07/2022