Complete Health Indicator Report of Depression: Adult Prevalence
Definition
The percentage of adults aged 18 and above who have ever been told by a doctor, nurse, or other health professionals that they have a depressive disorder, including depression, major depression, dysthymia, or minor depression.Numerator
The number of adults aged 18 and above who have ever been told by a doctor, nurse, or other health professional that they have a depressive disorder, including depression, major depression, dysthymia, or minor depression.Denominator
Adults aged 18 and above.Data Interpretation Issues
Question Text: "Has a doctor, nurse, or other health professional EVER told you that you have a depressive disorder, including depression, major depression, dysthymia, or minor depression?" NOTE: The question asks about lifetime diagnosis and does not reflect current major depression. As with all surveys, some error results from nonresponse (e.g., refusal to participate in the survey or to answer specific questions), and measurement (e.g., social desirability or recall bias). Error was minimized by use of strict calling protocols, good questionnaire design, standardization of interviewer behavior, interviewer training, and frequent, on-site interviewer monitoring and supervision.Why Is This Important?
Approximately 21.0%* of adults in the U.S. experienced some kind of mental illness during 2020^1^. Mental disorders like depression and anxiety can affect people's ability to take part in healthy behaviors. Similarly, physical health problems can make it harder for people to get treatment for mental disorders. Increasing screening for mental disorders can help people get the treatment they need^2^. Approximately 8.4% of adults suffered from at least one episode of major depression in 2020^3^. Major depression is defined as having severe symptoms that interfere with a person's ability to work, sleep, study, eat, and enjoy life. Symptoms of major depression may include fatigue or loss of energy, feelings of worthlessness or guilt, impaired concentration, loss of interest in daily activities, appetite or weight changes, sleep changes, and recurring thoughts of death or suicide. Despite the availability of effective treatments for major depression, such as medications and/or psychotherapeutic techniques, it often goes unrecognized and untreated.^4^[[br]] [[br]] ---- 1. National Institute of Mental Health. ''Any Mental Illness (AMI) Among U.S. Adults''. Retrieved from [https://www.nimh.nih.gov/health/statistics/mental-illness.shtml] on October 18, 2022. [[br]] 2. U.S. Department of Health and Human Services. ''Healthy People 2030''. With Understanding and Improving Health and Objectives for Improving Health. Washington, DC: U.S. Government Printing Office, November 2000 [https://health.gov/healthypeople/objectives-and-data/browse-objectives/mental-health-and-mental-disorders].[[br]] 3. National Institute of Mental Health. ''Major Depression Among Adults''. Retrieved from [https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adults.shtml] on October 18, 2022. [[br]] 4. National Alliance on Mental Illness Retrieved from [http://www.nami.org/Learn-More/Mental-Health-Conditions/Depression] on October 18, 2022.Other Objectives
Related to Healthy People 2030 Objective MHMD-11: Increase depression screening by primary care providers.How Are We Doing?
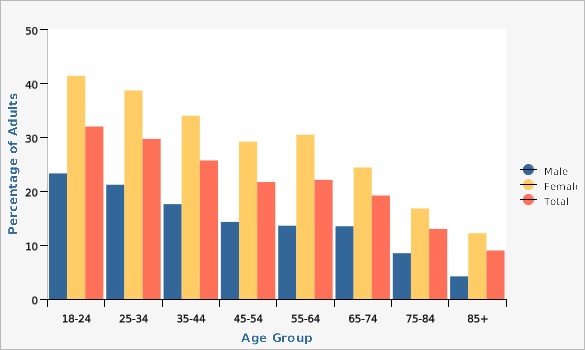
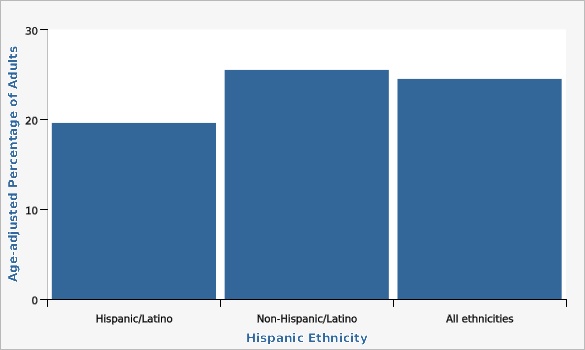
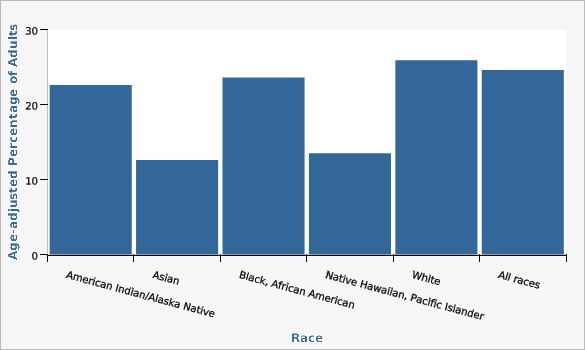
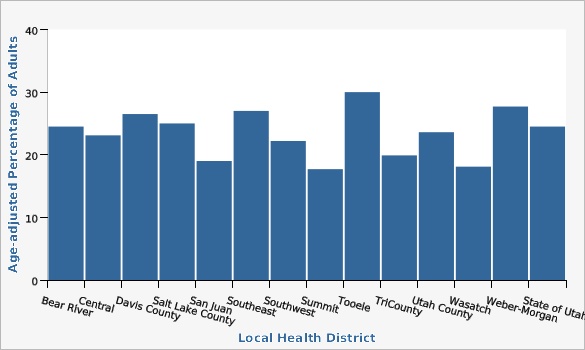
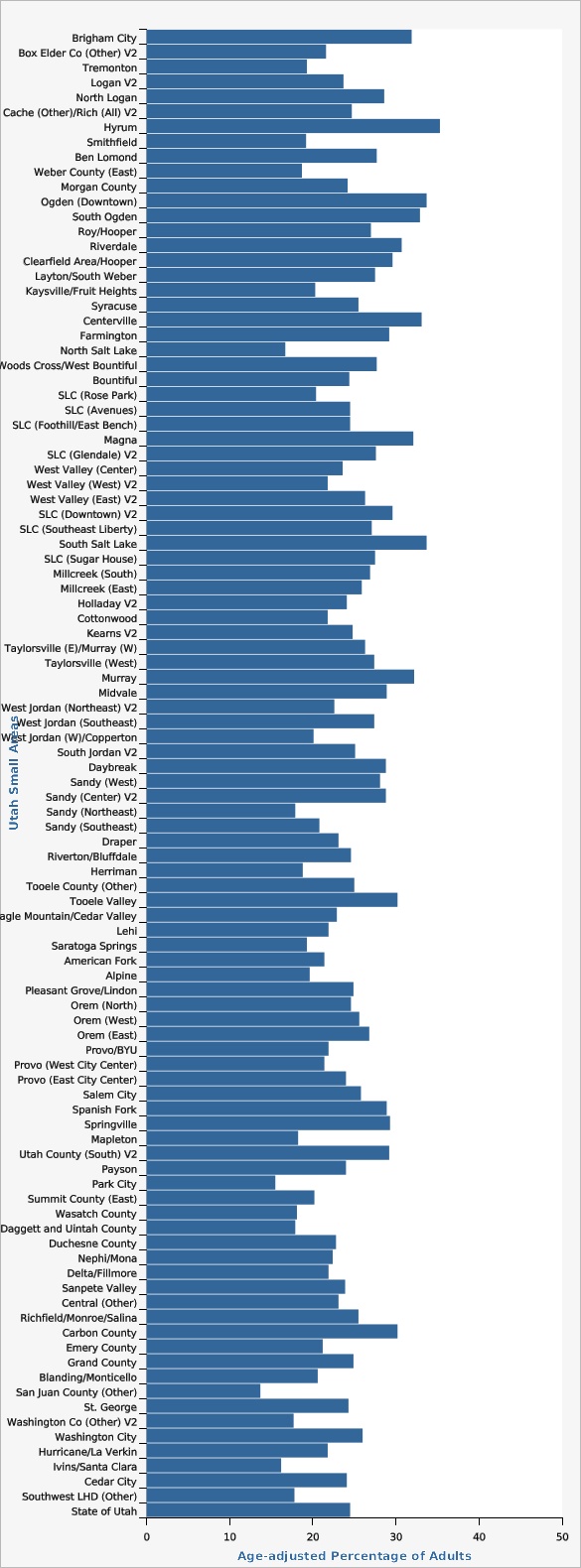
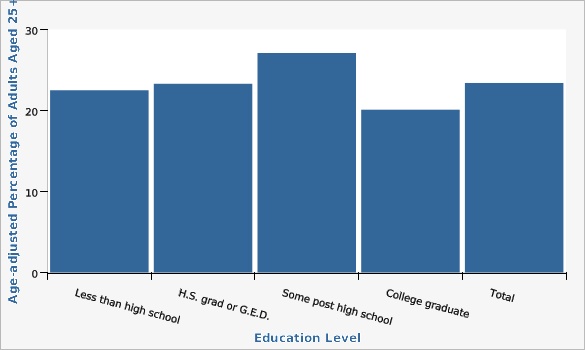
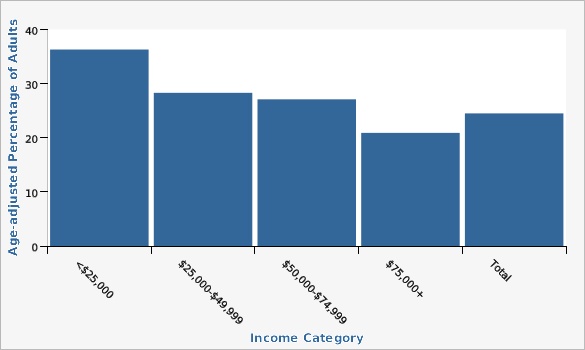
In Utah, adult women (34.3%) had significantly higher rates of doctor-diagnosed depression than men (18.1%) in 2022 (age-adjusted rates). Combined years 2020-2022 Utah data showed the following: * Hispanic (19.6%), Asian (12.6%), and Pacific Islander (13.5%) adults reported lower lifetime depression than the state rate. * Adults with a household income less than $25,000 (36.3%), those with a household income $25,000-$49,999 (28.3%), and those with a household income of $50,000-$74,999 (27.1%) had significantly higher rates of lifetime doctor-diagnosed depression, while adults with an income greater than $75,000 (20.9%) had lower rates of lifetime depression. * Depression also varied by education. Utah adults aged 25 and above with some post high school education but not a college degree (27.1%) had a higher rate of doctor-diagnosed depression compared to the state while Utah adults aged 25 and above with a college education (20.1%) had a lower rate of doctor-diagnosed depression. * Adults in TriCounty (19.9%) Wasatch (18.1%), and Summit County (17.7%) local health districts reported lower rates of doctor-diagnosed depression than the state rate. Davis County (26.5%), Tooele County (30.0%) and Weber-Morgan (27.7%) had a rate significantly higher than the state rate. * Among Utah Small Areas, Brigham City (31.9%), Ogden (Downtown) (33.7%), South Ogden (32.9%), Clearfield Area/Hooper (29.6%), Magna (32.1%), South Salt Lake (33.7%), Murray (32.2%), Tooele Valley (30.2%), and Carbon County (30.2%) had higher rates of doctor-diagnosed depression than the state rate. Weber County (East) (18.7%), Herriman (18.8%), Park City (15.5%), Wasatch County (18.1%), Daggett and Uintah County (17.9%), and San Juan (Other) (13.7%) had lower rates than the state rate.How Do We Compare With the U.S.?
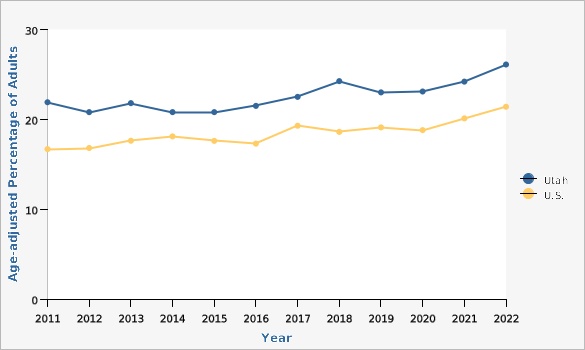
Utah has consistently higher rates of self-reported lifetime depression than the U.S. rate (26.1% vs. 21.4% in 2022).What Is Being Done?
The Utah Department of Health and Human Services, Office of Substance Use and Mental Health (OSUMH) facilitates the Utah Suicide Prevention Coalition. OSUMH grants funds to five local health or mental health authorities to design and implement comprehensive suicide prevention, intervention and postvention services. Comprehensive suicide prevention activities include promoting mental health resources and help-seeking behavior, distributing gun locks to reduce access to lethal means, development of community postvention plans, and training the community in suicide prevention using evidence-based/promising practice programs such as Question, Persuade, Refer (QPR), VitalCog (Workplace, Construction and Athletics), Mental Health First Aid, Safe and Effective Messaging for Suicide Prevention, and SafeTALK. These trainings promote knowledge and skill development for participants to recognize the warning signs of suicide, how to offer hope, and how to refer to resources and save a life. Additionally OSUMH grants funds to the remaining eight local health or mental health authorities to implement firearm/means safety programming within their areas. OSUMH also coordinates and funds many crisis services across the state, including 988 suicide and crisis lifeline, mobile crisis outreach teams (MCOT), stabilization and mobile response (SMR), and receiving centers.Evidence-based Practices
Evidence based practices for suicide prevention and media messaging can be found on [https://vipp.health.utah.gov/suicide-prevention/].Available Services
The Utah Department of Human Services Office of Substance Use and Mental Health (OSUMH) is the state agency responsible for ensuring that mental health services are available statewide. The Office also acts as a resource by providing general information, research results, and statistics to the public regarding substances of use and misuse and mental health services. The Office contracts with local mental health authorities to provide these services and monitors these LMHAs through site visits, a year-end review process, and a peer review process. Address:[[br]] Department of Health and Human Services[[br]] Office of Substance Use and Mental Health[[br]] 195 North 1950 West[[br]] Salt Lake City, UT 84116 Phone: (801) 538-3939[[br]] Fax: (801) 538-9892[[br]] [https://sumh.utah.gov/]Related Indicators
Relevant Population Characteristics
The proportion of adults who reported ever being told they had a depressive disorder varies by a number of population characteristics including age, sex, income, and education.Related Relevant Population Characteristics Indicators:
- Utah Population Characteristics: Age Distribution of the Population
- Utah Population Characteristics: Education Level in the Population
- Utah Population Characteristics: Household Income
- Utah Population Characteristics: Income per Capita
- Utah Population Characteristics: Poverty, All Persons
- Utah Population Characteristics: Racial and Ethnic Composition of the Population
Health Care System Factors
Because people with chronic health conditions may also be at greater risk for depression, it is important that primary care providers assess their patients with chronic physical conditions for depression. The Patient Health Questionnaire (PHQ-9) was developed to be used by primary care providers for screening, diagnosing, and measuring the severity of depression. The PHQ-9 was adapted for telephone health surveys and is asked on the Utah Behavioral Risk Factor Surveillance in some years.^1^[[br]] [[br]] ---- 1. Utah Health Status Update: Major Depression, October 2014, Utah Department of Health, available at: [https://ibis.health.utah.gov/pdf/opha/publication/hsu/2014/1410_Depression.pdf]Related Health Care System Factors Indicators:
Risk Factors
Utah adults who reported chronic illnesses and/or poor health status in general, were also more likely to have reported having ever been told they had a depressive disorder. It is known that behavioral health problems often co-occur with chronic diseases and may exacerbate poor health outcomes.Related Risk Factors Indicators:
Health Status Outcomes
In attempts to deal with the pain of depression, some people with depression turn to drugs, alcohol, and other harmful behaviors that can endanger their lives.Related Health Status Outcomes Indicators:
Graphical Data Views
| Utah vs. U.S. | Year | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | ||
|---|---|---|---|---|---|---|
Record Count: 24 | ||||||
| Utah | 2011 | 21.9% | 21.0% | 22.9% | ||
| Utah | 2012 | 20.8% | 19.9% | 21.8% | ||
| Utah | 2013 | 21.8% | 20.9% | 22.7% | ||
| Utah | 2014 | 20.8% | 20.0% | 21.6% | ||
| Utah | 2015 | 20.8% | 19.9% | 21.8% | ||
| Utah | 2016 | 21.5% | 20.5% | 22.6% | ||
| Utah | 2017 | 22.5% | 21.5% | 23.6% | ||
| Utah | 2018 | 24.2% | 23.2% | 25.3% | ||
| Utah | 2019 | 23.0% | 22.0% | 24.0% | ||
| Utah | 2020 | 23.1% | 22.1% | 24.2% | ||
| Utah | 2021 | 24.2% | 23.1% | 25.2% | ||
| Utah | 2022 | 26.1% | 25.0% | 27.3% | ||
| U.S. | 2011 | 16.7% | 16.5% | 16.9% | ||
| U.S. | 2012 | 16.8% | 16.6% | 17.0% | ||
| U.S. | 2013 | 17.6% | 17.4% | 17.8% | ||
| U.S. | 2014 | 18.1% | 17.9% | 18.3% | ||
| U.S. | 2015 | 17.6% | 17.4% | 17.8% | ||
| U.S. | 2016 | 17.3% | 17.0% | 17.6% | ||
| U.S. | 2017 | 19.3% | 19.0% | 19.5% | ||
| U.S. | 2018 | 18.6% | 18.4% | 18.8% | ||
| U.S. | 2019 | 19.1% | 18.8% | 19.3% | ||
| U.S. | 2020 | 18.8% | 18.5% | 19.1% | ||
| U.S. | 2021 | 20.1% | 19.8% | 20.3% | ||
| U.S. | 2022 | 21.4% | 21.1% | 21.6% | ||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression. [[br]] [[br]] Age-adjusted to the 2000 U.S. standard population. [[br]] Age-adjustment groups were 18-24, 25-34, 35-44, 45-64, 65+.Data Sources
- Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]
- Behavioral Risk Factor Surveillance System Survey Data, US Department of Health and Human Services Centers for Disease Control and Prevention (CDC).
| Males vs. Females | Age Group | Percentage of Adults | Lower Limit | Upper Limit | ||
|---|---|---|---|---|---|---|
Record Count: 24 | ||||||
| Male | 18-24 | 23.3% | 20.8% | 26.0% | ||
| Male | 25-34 | 21.2% | 19.2% | 23.2% | ||
| Male | 35-44 | 17.6% | 16.0% | 19.3% | ||
| Male | 45-54 | 14.3% | 12.7% | 16.1% | ||
| Male | 55-64 | 13.6% | 12.0% | 15.3% | ||
| Male | 65-74 | 13.5% | 11.9% | 15.4% | ||
| Male | 75-84 | 8.5% | 6.7% | 10.8% | ||
| Male | 85+ | 4.2% | 2.6% | 6.8% | ||
| Female | 18-24 | 41.4% | 38.1% | 44.7% | ||
| Female | 25-34 | 38.7% | 36.3% | 41.3% | ||
| Female | 35-44 | 34.0% | 31.8% | 36.2% | ||
| Female | 45-54 | 29.2% | 27.1% | 31.5% | ||
| Female | 55-64 | 30.5% | 28.2% | 32.8% | ||
| Female | 65-74 | 24.4% | 22.3% | 26.6% | ||
| Female | 75-84 | 16.8% | 14.5% | 19.4% | ||
| Female | 85+ | 12.2% | 9.2% | 16.1% | ||
| Total | 18-24 | 32.0% | 29.9% | 34.1% | ||
| Total | 25-34 | 29.7% | 28.1% | 31.4% | ||
| Total | 35-44 | 25.7% | 24.3% | 27.1% | ||
| Total | 45-54 | 21.7% | 20.3% | 23.1% | ||
| Total | 55-64 | 22.1% | 20.7% | 23.6% | ||
| Total | 65-74 | 19.2% | 17.8% | 20.6% | ||
| Total | 75-84 | 13.0% | 11.4% | 14.7% | ||
| Total | 85+ | 9.0% | 7.0% | 11.5% | ||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression.Data Source
Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]| Hispanic Ethnicity | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 3 | ||||||
| Hispanic/Latino | 19.6% | 17.9% | 21.4% | |||
| Non-Hispanic/Latino | 25.5% | 24.8% | 26.2% | |||
| All ethnicities | 24.5% | 23.9% | 25.1% | |||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression. [[br]] Age-adjusted to the 2000 U.S. standard population. [[br]]Data Source
Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]| Race | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 6 | ||||||
| American Indian/Alaska Native | 22.6% | 18.0% | 28.0% | |||
| Asian | 12.6% | 9.2% | 17.0% | |||
| Black, African American | 23.6% | 18.2% | 30.0% | |||
| Native Hawaiian, Pacific Islander | 13.5% | 8.8% | 20.2% | |||
| White | 25.9% | 25.2% | 26.5% | |||
| All races | 24.6% | 23.9% | 25.2% | |||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression. [[br]] [[br]] Age-adjusted to the 2000 U.S. standard population using three age groups (18-34, 35-49, 50+).Data Source
Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]| Local Health District | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 14 | ||||||
| Bear River | 24.5% | 22.2% | 27.1% | |||
| Central | 23.1% | 20.2% | 26.2% | |||
| Davis County | 26.5% | 24.5% | 28.6% | |||
| Salt Lake County | 25.0% | 23.9% | 26.1% | |||
| San Juan | 19.0% | 14.2% | 25.1% | |||
| Southeast | 27.0% | 23.2% | 31.3% | |||
| Southwest | 22.2% | 19.9% | 24.7% | |||
| Summit | 17.7% | 13.6% | 22.7% | |||
| Tooele | 30.0% | 26.7% | 33.5% | |||
| TriCounty | 19.9% | 17.0% | 23.1% | |||
| Utah County | 23.6% | 22.2% | 24.9% | |||
| Wasatch | 18.1% | 14.1% | 23.0% | |||
| Weber-Morgan | 27.7% | 25.5% | 30.0% | |||
| State of Utah | 24.5% | 23.9% | 25.1% | |||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression. [[br]] Age-adjusted to the 2000 standard U.S. population.Data Source
Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]| Utah Small Areas | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | Note | ||
|---|---|---|---|---|---|---|
Record Count: 100 | ||||||
| Brigham City | 31.9% | 25.4% | 39.3% | |||
| Box Elder Co (Other) V2 | 21.6% | 14.6% | 30.9% | |||
| Tremonton | 19.3% | 13.2% | 27.3% | |||
| Logan V2 | 23.7% | 19.4% | 28.6% | |||
| North Logan | 28.6% | 21.8% | 36.5% | |||
| Cache (Other)/Rich (All) V2 | 24.7% | 18.6% | 31.9% | |||
| Hyrum | 35.3% | 23.9% | 48.6% | |||
| Smithfield | 19.2% | 12.6% | 28.2% | |||
| Ben Lomond | 27.7% | 23.3% | 32.6% | |||
| Weber County (East) | 18.7% | 14.2% | 24.3% | |||
| Morgan County | 24.2% | 16.0% | 34.9% | |||
| Ogden (Downtown) | 33.7% | 28.1% | 39.7% | |||
| South Ogden | 32.9% | 27.3% | 39.0% | |||
| Roy/Hooper | 27.0% | 22.0% | 32.7% | |||
| Riverdale | 30.7% | 23.3% | 39.2% | |||
| Clearfield Area/Hooper | 29.6% | 25.0% | 34.7% | |||
| Layton/South Weber | 27.5% | 23.5% | 32.0% | |||
| Kaysville/Fruit Heights | 20.3% | 15.4% | 26.2% | |||
| Syracuse | 25.5% | 19.5% | 32.5% | |||
| Centerville | 33.1% | 24.0% | 43.7% | |||
| Farmington | 29.2% | 21.6% | 38.1% | |||
| North Salt Lake | 16.7% | 10.9% | 24.7% | |||
| Woods Cross/West Bountiful | 27.7% | 19.7% | 37.4% | |||
| Bountiful | 24.4% | 19.5% | 30.1% | |||
| SLC (Rose Park) | 20.4% | 14.7% | 27.6% | |||
| SLC (Avenues) | 24.5% | 17.7% | 32.9% | |||
| SLC (Foothill/East Bench) | 24.5% | 17.2% | 33.5% | |||
| Magna | 32.1% | 25.4% | 39.7% | |||
| SLC (Glendale) V2 | 27.6% | 19.5% | 37.3% | |||
| West Valley (Center) | 23.6% | 18.6% | 29.5% | |||
| West Valley (West) V2 | 21.8% | 16.2% | 28.6% | |||
| West Valley (East) V2 | 26.3% | 21.4% | 32.0% | |||
| SLC (Downtown) V2 | 29.6% | 23.7% | 36.2% | |||
| SLC (Southeast Liberty) | 27.1% | 20.5% | 35.0% | |||
| South Salt Lake | 33.7% | 26.4% | 41.7% | |||
| SLC (Sugar House) | 27.5% | 21.8% | 34.0% | |||
| Millcreek (South) | 26.9% | 19.2% | 36.3% | |||
| Millcreek (East) | 25.9% | 19.3% | 33.7% | |||
| Holladay V2 | 24.1% | 17.9% | 31.6% | |||
| Cottonwood | 21.8% | 16.4% | 28.4% | |||
| Kearns V2 | 24.8% | 19.4% | 31.1% | |||
| Taylorsville (E)/Murray (W) | 26.3% | 20.6% | 32.9% | |||
| Taylorsville (West) | 27.4% | 21.9% | 33.8% | |||
| Murray | 32.2% | 26.0% | 39.0% | |||
| Midvale | 28.9% | 22.8% | 35.9% | |||
| West Jordan (Northeast) V2 | 22.6% | 17.1% | 29.2% | |||
| West Jordan (Southeast) | 27.4% | 21.5% | 34.1% | |||
| West Jordan (W)/Copperton | 20.1% | 15.2% | 26.2% | |||
| South Jordan V2 | 25.1% | 19.2% | 32.1% | |||
| Daybreak | 28.8% | 22.7% | 35.9% | |||
| Sandy (West) | 28.1% | 21.1% | 36.3% | |||
| Sandy (Center) V2 | 28.8% | 21.7% | 37.0% | |||
| Sandy (Northeast) | 17.9% | 11.5% | 27.0% | |||
| Sandy (Southeast) | 20.8% | 15.8% | 26.8% | |||
| Draper | 23.1% | 17.8% | 29.5% | |||
| Riverton/Bluffdale | 24.6% | 20.0% | 29.9% | |||
| Herriman | 18.8% | 14.9% | 23.5% | |||
| Tooele County (Other) | 25.0% | 18.3% | 33.3% | |||
| Tooele Valley | 30.2% | 26.5% | 34.2% | |||
| Eagle Mountain/Cedar Valley | 22.9% | 17.5% | 29.4% | |||
| Lehi | 21.9% | 18.1% | 26.3% | |||
| Saratoga Springs | 19.3% | 14.3% | 25.6% | |||
| American Fork | 21.4% | 17.2% | 26.4% | |||
| Alpine | 19.6% | 10.4% | 34.0% | * | ||
| Pleasant Grove/Lindon | 24.9% | 20.6% | 29.6% | |||
| Orem (North) | 24.6% | 19.3% | 30.7% | |||
| Orem (West) | 25.6% | 21.0% | 30.8% | |||
| Orem (East) | 26.8% | 20.3% | 34.4% | |||
| Provo/BYU | 21.9% | 17.2% | 27.5% | |||
| Provo (West City Center) | 21.4% | 16.5% | 27.4% | |||
| Provo (East City Center) | 24.0% | 17.3% | 34.2% | |||
| Salem City | 25.8% | 16.8% | 37.5% | |||
| Spanish Fork | 28.9% | 23.3% | 35.1% | |||
| Springville | 29.3% | 23.8% | 35.5% | |||
| Mapleton | 18.2% | 11.2% | 28.3% | * | ||
| Utah County (South) V2 | 29.2% | 21.1% | 39.0% | |||
| Payson | 24.0% | 18.3% | 30.9% | |||
| Park City | 15.5% | 10.8% | 21.8% | |||
| Summit County (East) | 20.2% | 14.1% | 27.9% | |||
| Wasatch County | 18.1% | 14.1% | 23.0% | |||
| Daggett and Uintah County | 17.9% | 14.9% | 21.4% | |||
| Duchesne County | 22.8% | 17.9% | 28.6% | |||
| Nephi/Mona | 22.4% | 14.4% | 33.0% | |||
| Delta/Fillmore | 21.9% | 14.4% | 31.8% | |||
| Sanpete Valley | 23.9% | 18.2% | 30.8% | |||
| Central (Other) | 23.1% | 18.0% | 29.2% | |||
| Richfield/Monroe/Salina | 25.5% | 19.7% | 32.3% | |||
| Carbon County | 30.2% | 25.2% | 35.7% | |||
| Emery County | 21.2% | 14.7% | 29.7% | |||
| Grand County | 24.9% | 17.3% | 34.4% | |||
| Blanding/Monticello | 20.6% | 14.6% | 28.1% | |||
| San Juan County (Other) | 13.7% | 7.2% | 24.4% | |||
| St. George | 24.3% | 20.4% | 28.6% | |||
| Washington Co (Other) V2 | 17.7% | 9.9% | 29.6% | |||
| Washington City | 26.0% | 18.5% | 35.4% | |||
| Hurricane/La Verkin | 21.8% | 14.8% | 31.0% | |||
| Ivins/Santa Clara | 16.2% | 9.0% | 27.2% | |||
| Cedar City | 24.1% | 19.2% | 29.2% | |||
| Southwest LHD (Other) | 17.8% | 12.4% | 25.0% | |||
| State of Utah | 24.5% | 23.9% | 25.1% | |||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression. [[br]] [[br]] Age-adjusted to the 2000 U.S. standard population. *Use caution in interpreting data for Alpine and Mapleton small areas; the estimate has a coefficient of variation > 30% and is therefore deemed unreliable by Utah Department of Health and Human Services standards. A description of the Utah Small Areas may be found on IBIS at the following URL: [https://ibis.health.utah.gov/resource/Guidelines.html].Data Source
Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]| Education Level | Age-adjusted Percentage of Adults Aged 25+ | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 5 | ||||||
| Less than high school | 22.5% | 19.7% | 25.5% | |||
| H.S. grad or G.E.D. | 23.3% | 22.0% | 24.6% | |||
| Some post high school | 27.1% | 25.9% | 28.3% | |||
| College graduate | 20.1% | 19.2% | 21.0% | |||
| Total | 23.4% | 22.8% | 24.0% | |||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression. [[br]] [[br]]Age-adjusted to the 2000 U.S. standard population.Data Source
Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]| Income Category | Age-adjusted Percentage of Adults | Lower Limit | Upper Limit | |||
|---|---|---|---|---|---|---|
Record Count: 5 | ||||||
| <$25,000 | 36.3% | 33.9% | 38.7% | |||
| $25,000-$49,999 | 28.3% | 26.7% | 29.9% | |||
| $50,000-$74,999 | 27.1% | 25.5% | 28.9% | |||
| $75,000+ | 20.9% | 19.9% | 21.9% | |||
| Total | 24.5% | 23.9% | 25.1% | |||
Data Notes
The question asks about lifetime diagnosis and does not reflect current major depression. [[br]] [[br]] Age-adjusted to the U.S. 2000 standard population.Data Source
Utah Department of Health and Human Services Behavioral Risk Factor Surveillance System (BRFSS) [https://ibis.health.utah.gov/ibisph-view/query/selection/brfss/BRFSSSelection.html]More Resources and Links
Evidence-based community health improvement ideas and interventions may be found at the following sites:- Centers for Disease Control and Prevention (CDC) WONDER Database, a system for disseminating public health data and information.
- United States Census Bureau data dashboard.
- Utah healthy Places Index, evidence-based and peer-reviewed tool, supports efforts to prioritize equitable community investments, develop critical programs and policies across the state, and much more.
- County Health Rankings
- Kaiser Family Foundation's StateHealthFacts.org
- Medical literature can be queried at PubMed library.
Page Content Updated On 02/29/2024,
Published on 03/22/2024