Why Is This Important?
Experience is not the same as satisfaction.
Patient experience surveys such as CAHPS sometimes are mistaken for customer satisfaction surveys. Patient experience surveys focus on how patients experienced or perceived key aspects of their care, not how satisfied they were with their care. Patient experience surveys such as CAHPS focus on asking patients whether or how often they experienced critical aspects of health care, including communication with their doctors, understanding their medication instructions, and the coordination of their health care needs. They do not focus on amenities.
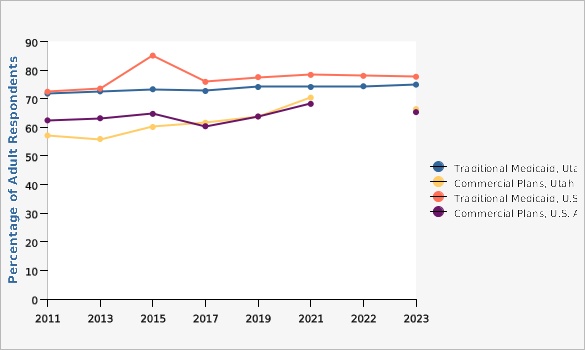
The Utah Department of Health and Human Services Office of Research and Evaluation implements and administers several different patient experience surveys. These surveys ask patients (or in some cases their families) about their experiences with, and ratings of, their health care providers and plans, including hospitals, home health care agencies, doctors, and health and drug plans, among others. The surveys focus on matters that patients themselves say are important to them and for which patients are the best and/or only source of information.Percentage of Enrollees in Medicaid or Commercial Health Plans Who Rated Their Health Plan Experience an 8, 9, or 10, Utah and U.S. Adults, 2011-2023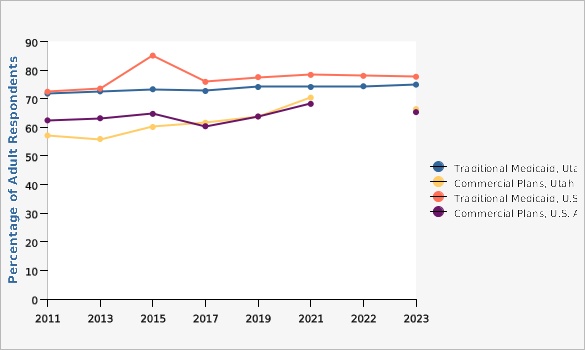 |
Data Source
Consumer Assessment of Health Plans Survey, Healthcare Information & Analysis Programs, Office of Research & Evaluation, Utah Department of Health and Human Services
Data Notes
Until 2021, odd-year surveys were for adult enrollees of Utah health plans, while the even-year surveys were for child enrollees. Starting in 2021, all Medicaid plans are reporting both their adult and child populations each year while commercial plans continue every other year. Medicaid is a source of health insurance coverage for Utah's vulnerable populations. Medicaid is a state and federal program that pays for medical services for low-income pregnant women, children, individuals who are elderly or have a disability, parents, and women with breast or cervical cancer. To qualify, these individuals must meet income and other eligibility requirements. Commercial health insurance is defined as any type of health benefit not obtained from Medicare or Medicaid plans. The insurance may be employer-sponsored or privately purchased. Commercial health insurance may be provided on a fee-for-service basis or through a managed care plan. [[br]]
[[br]] The percentage of respondents who rated their health plan experience an 8, 9, or 10 was calculated for Medicaid and commercial plans to derive the values presented. Values for commercial plans are available from 2015 forward. U.S. Averages are not available for commercial plans.What Is Being Done?
The Department of Health and Human Services Office of Research and Evaluation produces and releases a "Patient Experience Report of Utah Health Plans" every year with updated CAHPS survey results and other HEDIS (Healthcare Effectiveness Data and Information Set) measures. These can be viewed and downloaded at [https://stats.health.utah.gov/about-the-data/healthcare-facility-data/].
Date Indicator Content Last Updated: 02/29/2024