Complete Health Indicator Report of Newborn Hearing Screening
Definition
Screening for hearing loss for newborn infants has been mandated in Utah since 1998. Because half of the children with hearing loss have no family history of deafness or hearing loss, universal screening is conducted to detect children with permanent congenital hearing loss (PCHL) as soon as possible. There is substantial evidence that newborn hearing screening is highly accurate and leads to earlier identification and treatment of infants with hearing loss. Healthy People 2020 Objectives addressed in this report include: * HP 2020 ENT-VSL-1.1 Percentage of newborns who are screened for hearing loss no later than age 1 month. * HP 2020 ENT-VSL-1.2 Percentage of infants who did not pass hearing screening who received audiologic evaluation by age 3 months. * HP 2020 ENT-VSL-1.3 Percentage of infants with confirmed hearing loss enrolled in intervention services no later than age 6 months.Numerator
ENT-VSL-1.1 Number of newborns screened for hearing loss by one month of age[[br]] ENT-VSL-1.2 Number of newborns who received an audiologic evaluation following failed hearing screening[[br]] ENT-VSL-1.3 Number of infants with confirmed hearing loss enrolled in Early InterventionDenominator
ENT-VSL-1.1 Number of occurrent births in Utah[[br]] ENT-VSL-1.2 Number of infants referred for audiologic evaluation[[br]] ENT-VSL-1.3 Number of infants with confirmed permanent hearing lossWhy Is This Important?
It is extremely important for hearing loss to be detected early to optimize communication development. The most effective method to implement early identification of hearing loss is to screen all infants before they leave the birthing hospital or before ten days of age to diagnose permanent hearing loss quickly, and begin intervention as soon as possible.Other Objectives
{{style color:#003366 ENT-VSL-1.1:}} Increase the proportion of newborns who are screened for hearing loss no later than age 1 month * '''U.S. 2017 Baseline:''' 95.4 percent * '''Utah 2017 Baseline:''' 97.3 percent[[br]] Target to maintain > 95% by 2024.[[br]] [[br]] {{style color:#003366 ENT-VSL-1.2:}} Increase the proportion of newborns who receive audiologic evaluation no later than age 3 months for infants who did not pass the hearing screening * '''U.S. 2017 Baseline:''' 49.2 percent * '''Utah 2017 Baseline:''' 64.8 percent[[br]] Target by 2024 min of 85%, or increase by 10% from baseline.[[br]] [[br]] {{style color:#003366 ENT-VSL-1.3:}} Increase the proportion of infants with confirmed hearing loss who are enrolled for intervention services no later than age 6 months * '''U.S. 2017 Baseline:''' 43.4 percent * '''Utah 2017 Baseline:''' 68.4 percent Target by 2024 min of 80%, or to increase by 15% from baseline.[[br]] [[br]] Targets are from EHDI HRSA Grant 2020-2024.How Are We Doing?
The Utah Early Hearing Detection and Intervention (EHDI) Program within the Utah Department of Health and Human Services oversees newborn hearing screening in Utah and documents hearing screening on over 99% of newborns. In 2022, 97.3% of all infants born in the state of Utah received a hearing screening prior to one month of age. Of just those infants who received a screening, 98.5% were prior to 1 month (as reported to the CDC EHDI Hearing Screening and Follow-up Survey [HSFS]), an increase from 97.4% reported for 2011 births. Many of the infants with screening delayed past one month are NICU (newborn intensive care unit) infants where screening may not be indicated until discharge (often after one month of age), or home births who may not have access to screening before one month of age. Those infants who failed their most recent screening should have a diagnostic exam with a pediatric audiologist prior to 3 months of age. Infants who received a diagnostic exam prior to three months steadily increased from 19.2% in 2011 to 79.4% in 2022. For infants born in 2022 who received a diagnostic exam, 87.2% were prior to 3 months of age. Infants undergoing diagnostic procedures may receive confirmation of hearing loss after the optimal 3-month "window" although they received one or more diagnostic evaluations before that time. The values reported to the CDC are based on the final or "confirmed" hearing status which could include multiple previous diagnostic exams. Utah continues to have one of the lowest lost to follow-up rates in the nation, even throughout the COVID-19 pandemic, with 2021 overall lost to follow-up at 3.9% vs the national rate of 32.4% (national numbers for 2022 are not yet published).How Do We Compare With the U.S.?
In 2021, data from the Centers for Disease Control and Prevention (CDC) EHDI showed that 98% of newborns in the United States (48 states, 6 territories, 1 district) were screened for hearing loss, with 95.5% screened by one month of age. Of those infants not passing the hearing screening, 57.6% had a diagnostic evaluation; 42.7% were diagnosed as either having or not having a hearing loss before three months of age. Nationally, we saw a decrease in infants receiving a timely diagnostic exam due to the COVID-19 pandemic, however Utah remained steady, continuing to offer services throughout the pandemic. ''* For data tracking and reporting purposes, those "referred for evaluation" include all infants who did not pass their final hearing screening or went directly to evaluation with no screening. While Utah is a 2-stage screening state, this number includes all infants who did not pass both inpatient and outpatient screens and were referred for diagnostic audiology, as well as those infants who did not pass inpatient screening and did not return for outpatient screening.''[[br]] Of infants "referred for evaluation"* in 2021: * % with no loss ** U.S.: 65.4% ** Utah: 47.4% [[br]] *% with hearing loss ** U.S.: 10.3% ** Utah: 14.8% [[br]] *% overall loss to follow-up ** U.S.: 32.4% ** Utah: 3.9% [[br]] *% loss to follow-up due to "unable to contact/unknown" ** U.S.: 22.7% ** Utah: 0%[[br]] [[br]] *% loss to follow-up due to "contacted unresponsive" ** U.S.: 9.6% ** Utah: 3.9%[[br]] [[br]] National Early Hearing Detection and Intervention (EHDI) data shows that 67.1% of infants born in 2021 with hearing loss who are receiving EI (Early Intervention) services were enrolled prior to six months of age; Utah showed a 87.3% enrollment success rate by six months of age for 2021.[[br]] [[br]] ---- Data source: [https://www.cdc.gov/ncbddd/hearingloss/2021-data/documents/01-2021-HSFS-Data-Summary-h.pdf] Published November 2023.What Is Being Done?
State legislation requires that ALL newborns, including those born at home, must have their hearing screened by one month of age and results reported to the Utah Department of Health and Human Services. Increased efforts have been focused on providing screening equipment, support, and training for local midwives who collectively birth over 1,000 infants per year. The Utah Newborn Hearing Screening/EHDI Program supports tracking efforts and provides resource information to hospitals, midwives, medical providers, local programs, and families. Improvements in the EHDI tracking surveillance system and decreasing loss to follow-up/documentation has been a priority, as well as matching EHDI data across other state programs (Utah Birth Defects Network, Critical Congenital Heart Defect (CCHD) screening, Vital Records, etc.). Implementation of the Birth Certificate Alert Program, in collaboration with local health departments, began statewide in 2014. Twenty-six of 29 local health department birth certificate offices are now participating. Alerts to parents applying for their child's birth certificate are generated if their infant has not yet completed the newborn hearing screening process. The Newborn Hearing Screening Committee endorses Healthy People 2020/2030 goals and assesses progress quarterly. The Utah EHDI Program has been working extensively with the Office of Vital Records both to clean and match data, as well as by updating the Birth Certificate Application so that midwives can now enter (September 2020) newborn hearing screening results as they apply for the child's birth certificate. Beginning in 2017 the Utah EHDI Program partnered with Utah Family Voices/Utah Parent Center to employ Parent Consultants to provide support to families who have a child who is deaf or hard of hearing. This has been a valuable partnership providing support to families throughout Utah. Particular emphasis has been put on collaborating with Baby Watch Early Intervention and the Utah Schools for the Deaf and Blind Parent Infant Program to increase enrollment and education in regards to Early Intervention services. In-line with HRSA funding, the EHDI Program is also working to expand technical assistance to Early Childhood screening programs.Evidence-based Practices
The Utah EHDI program follows all of the best practice guidelines within this document: Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs [[br]] [https://digitalcommons.usu.edu/cgi/viewcontent.cgi?article=1104&context=jehdi]Available Services
Resources for families and providers on deafness and hearing loss, state requirements, intervention services, and related handouts are available at [https://familyhealth.utah.gov/ehdi]. For regional resources for hearing screening and diagnostic services for newborn and infants: [https://arcg.is/n4HmC] Families of infants identified with permanent hearing loss are offered targeted services for deaf and hard of hearing children birth through 3 years of age through the Baby Watch Early Intervention Program ([https://familyhealth.utah.gov/oec/baby-watch-early-intervention/ BWEIP]) and the Utah School for the Deaf Parent Infant Program ([https://www.usdb.org/programs/deaf-and-hard-of-hearing/ USDB]). Families in need of parent-to-parent support upon initial diagnosis or at any point throughout the EHDI process may contact EHDIparents@utah.gov. For up-to-date resources and community happenings, interested parties can follow the Utah EHDI Family Support and Information Facebook page (@UtahEHDI). The Utah Parent Center helps all families no matter their child's diagnosis. For more information, visit [https://utahparentcenter.org]. The Utah Children's Hearing Aid Program (CHAP) provides access to hearing aids to children 17 years of age or younger for financially eligible families. For more information and/or to apply, visit [https://familyhealth.utah.gov/CHAP].Related Indicators
Relevant Population Characteristics
All hospitals and birth attendants are required to participate in newborn hearing screening by legislative mandate. Hospital programs have screening equipment on site and do a very good job of screening babies prior to discharge. For babies who require follow-up, completion rates are dependent upon individual hospital commitment, location, and patient demographics. Actual screening rates for home births reflect local availability, cost, and convenience for families. Home birth hearing projects have increased out-of-hospital screening rates from 23% in 2007 to more than 95% in 2022.Related Relevant Population Characteristics Indicators:
Health Care System Factors
All hospitals are required to participate in newborn hearing screening by legislative mandate. However, actual screening rates and timelines are dependent upon individual hospital commitment, regardless of demographics.Related Health Care System Factors Indicators:
Risk Factors
The National Joint Committee on Infant Hearing, Year 2007 Position Statement lists hearing risk factors which are addressed by Utah newborn hearing programs. [http://www.cdc.gov/ncbddd/hearingloss/documents/JCIH_2007.pdf] Appendix 2, Page 24.Related Risk Factors Indicators:
Health Status Outcomes
The critical age for initiating habilitation for hearing loss is prior to six months of age. Most infants receiving intervention by this age develop language and social skills approximating their normal hearing peers by kindergarten enrollment. Intervention delayed beyond six months has been shown to have less successful outcomes.Graphical Data Views
Newborn hearing screening ENT-VSL-1.1: Screening for hearing loss no later than age 1, month, Utah, 2010-2022
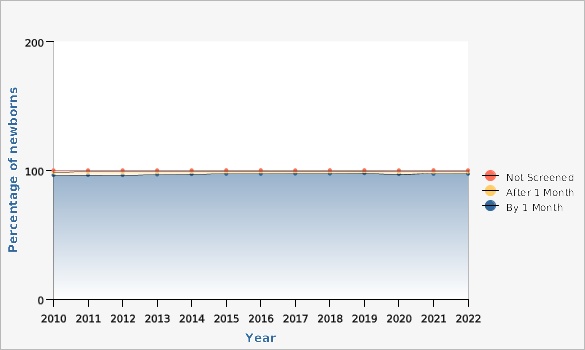
Screening for hearing loss is completed by hospital staff prior to discharge or for infants born outside a hospital setting by the attending midwife or other community provider. Screening is accomplished through automated auditory brainstem response (A-ABR) or otoacoustic emissions (OAE) in accordance with the Joint Committee on Infant Hearing (JCIH, 2019).
| Hearing Screening | Year | Percentage of newborns | ||||
|---|---|---|---|---|---|---|
Record Count: 39 | ||||||
| By 1 Month | 2010 | 96.2% | ||||
| By 1 Month | 2011 | 96.3% | ||||
| By 1 Month | 2012 | 96.2% | ||||
| By 1 Month | 2013 | 96.7% | ||||
| By 1 Month | 2014 | 97.0% | ||||
| By 1 Month | 2015 | 97.2% | ||||
| By 1 Month | 2016 | 97.2% | ||||
| By 1 Month | 2017 | 97.4% | ||||
| By 1 Month | 2018 | 97.4% | ||||
| By 1 Month | 2019 | 97.7% | ||||
| By 1 Month | 2020 | 97.0% | ||||
| By 1 Month | 2021 | 97.2% | ||||
| By 1 Month | 2022 | 97.3% | ||||
| After 1 Month | 2010 | 2.4% | ||||
| After 1 Month | 2011 | 2.5% | ||||
| After 1 Month | 2012 | 2.6% | ||||
| After 1 Month | 2013 | 2.2% | ||||
| After 1 Month | 2014 | 1.9% | ||||
| After 1 Month | 2015 | 1.9% | ||||
| After 1 Month | 2016 | 2.0% | ||||
| After 1 Month | 2017 | 1.8% | ||||
| After 1 Month | 2018 | 1.7% | ||||
| After 1 Month | 2019 | 1.6% | ||||
| After 1 Month | 2020 | 1.7% | ||||
| After 1 Month | 2021 | 1.5% | ||||
| After 1 Month | 2022 | 1.4% | ||||
| Not Screened | 2010 | 1.4% | ||||
| Not Screened | 2011 | 1.2% | ||||
| Not Screened | 2012 | 1.2% | ||||
| Not Screened | 2013 | 1.1% | ||||
| Not Screened | 2014 | 1.1% | ||||
| Not Screened | 2015 | 0.9% | ||||
| Not Screened | 2016 | 0.8% | ||||
| Not Screened | 2017 | 0.8% | ||||
| Not Screened | 2018 | 0.9% | ||||
| Not Screened | 2019 | 0.7% | ||||
| Not Screened | 2020 | 1.3% | ||||
| Not Screened | 2021 | 1.3% | ||||
| Not Screened | 2022 | 1.3% | ||||
Data Notes
New hearing screening objectives adopted in 2010 therefore trend data begins in 2010. Changes in CDC HSFS reporting were implemented in 2020. These changes count infants who were not screened but went directly for a diagnostic evaluation as missed, where historically these infants were counted as "Screened - not passed". This causes the "not screened" numbers to be higher from 2020 on. Infants should be screened by 1 month of age. Infants not screened include infants who are deceased, refused screening, or are lost to follow-up.Data Source
NBHS - HI*TRACK Hearing Screening Tracking and Data Management (C) HI*TRACK, Utah State UniversityNewborn hearing screening ENT-VSL-1.2: Infants receiving audiologic evaluation following failed hearing screening, Utah, 2010-2022
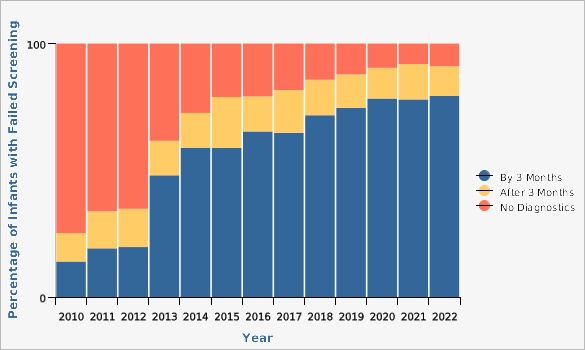
When an infant does not pass newborn hearing screening the infant is referred to an audiologist with expertise in infant testing to perform a diagnostic audiologic evaluation. The diagnostic testing should be performed no later than 3 months of age.
| Timely Diagnostic Evaluation | Year | Percentage of Infants with Failed Screening | ||||
|---|---|---|---|---|---|---|
Record Count: 39 | ||||||
| By 3 Months | 2010 | 14.0% | ||||
| By 3 Months | 2011 | 19.2% | ||||
| By 3 Months | 2012 | 19.7% | ||||
| By 3 Months | 2013 | 48.0% | ||||
| By 3 Months | 2014 | 58.9% | ||||
| By 3 Months | 2015 | 58.8% | ||||
| By 3 Months | 2016 | 65.3% | ||||
| By 3 Months | 2017 | 64.8% | ||||
| By 3 Months | 2018 | 71.7% | ||||
| By 3 Months | 2019 | 74.6% | ||||
| By 3 Months | 2020 | 78.3% | ||||
| By 3 Months | 2021 | 77.9% | ||||
| By 3 Months | 2022 | 79.4% | ||||
| After 3 Months | 2010 | 11.2% | ||||
| After 3 Months | 2011 | 14.6% | ||||
| After 3 Months | 2012 | 15.1% | ||||
| After 3 Months | 2013 | 13.6% | ||||
| After 3 Months | 2014 | 13.7% | ||||
| After 3 Months | 2015 | 20.1% | ||||
| After 3 Months | 2016 | 13.8% | ||||
| After 3 Months | 2017 | 16.8% | ||||
| After 3 Months | 2018 | 14.0% | ||||
| After 3 Months | 2019 | 13.2% | ||||
| After 3 Months | 2020 | 12.1% | ||||
| After 3 Months | 2021 | 14.0% | ||||
| After 3 Months | 2022 | 11.6% | ||||
| No Diagnostics | 2010 | 74.8% | ||||
| No Diagnostics | 2011 | 66.2% | ||||
| No Diagnostics | 2012 | 65.2% | ||||
| No Diagnostics | 2013 | 38.4% | ||||
| No Diagnostics | 2014 | 27.4% | ||||
| No Diagnostics | 2015 | 21.1% | ||||
| No Diagnostics | 2016 | 20.9% | ||||
| No Diagnostics | 2017 | 18.4% | ||||
| No Diagnostics | 2018 | 14.3% | ||||
| No Diagnostics | 2019 | 12.2% | ||||
| No Diagnostics | 2020 | 9.6% | ||||
| No Diagnostics | 2021 | 8.1% | ||||
| No Diagnostics | 2022 | 9.0% | ||||
Data Notes
New hearing screening objectives adopted in 2010 therefore trend data begins in 2010. Approximately 1% of all Utah births require diagnostic follow-up for not passing the newborn hearing screening 2-stage process. Not showing on this graph is that the Utah lost to follow-up rate has also decreased from 67.0% in 2010 to 0% in 2022.[[br]] [[br]] Reasons for not having a diagnostic exam are broken out in [[a href="indicator/view/NewHearScr.EvalReas.html" ENT-VSL-1.2 (Part 2): Reasons for No Diagnosis]].Data Source
NBHS - HI*TRACK Hearing Screening Tracking and Data Management (C) HI*TRACK, Utah State UniversityNewborn hearing screening ENT-VSL-1.2 (Part 2): Reasons for no diagnosis, Utah, 2010-2022
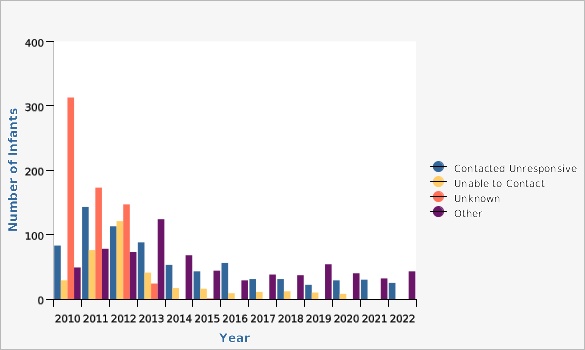
The Utah lost to follow-up (LTFU) number consists of those children who are "contacted unresponsive", "unable to contact", and "unknown". However, there are many reasons that families do not follow-up for services. Those "other" include: "in process" (e.g., need pressure equalization tubes for chronic middle ear fluid or on cleft palate repair, etc.), non-resident, moved out of jurisdiction, unable to receive due to medical reasons, primary care physician did not refer, infant died, or the family declined. In 2014 the CDC gave states the option to remove "contacted but unresponsive" from their LTFU numbers, due to the fact that someone within the EHDI system has had 2-way communication with the family and they chose to not follow-up. For both 2021 and 2022, this would give Utah a LTFU rate of 0% (no infants were "unable to contact" or "unknown").
The CDC defines LTFU categories as follows: "contacted unresponsive" - "a documented two-way conversation or written communication with the child's legal parent or guardian in which they have acknowledged awareness and have nevertheless not obtained the recommended service"; "unable to contact" - "the parents or family were not able to be contacted because the EHDI program/hospital/provider did not have any current/correct contact information"; "unknown" - "there is no documentation that they received any follow-up testing and there has been no documented contact with the parents".
Not showing on this graph is that the Utah LTFU rate has decreased in recent years.
*2010: 67.0%
*2011: 55.2%
*2012: 54.7%
*2013: 31.1%
*2014: 13.9%/3.4% removing "parent contacted unresponsive"
*2015: 12.2%/3.4% removing "parent contacted unresponsive"
*2016: 14.5%/2.0% removing "parent contacted unresponsive"
*2017: 9.7%/2.5% removing "parent contacted unresponsive"
*2018: 7.7%/2.1% removing "parent contacted unresponsive"
*2019: 4.5%/1.4% removing "parent contacted unresponsive"
*2020: 4.6%/1.0% removing "parent contacted unresponsive"
*2021: 3.9%/0.0% removing "parent contacted unresponsive"
*2022: 3.3%/0.0% removing "parent contacted unresponsive" [[br]]
[[br]]
| Reasons for No Diagnosis | Year | Number of Infants | ||||
|---|---|---|---|---|---|---|
Record Count: 52 | ||||||
| Contacted Unresponsive | 2010 | 83 | ||||
| Contacted Unresponsive | 2011 | 143 | ||||
| Contacted Unresponsive | 2012 | 113 | ||||
| Contacted Unresponsive | 2013 | 88 | ||||
| Contacted Unresponsive | 2014 | 53 | ||||
| Contacted Unresponsive | 2015 | 43 | ||||
| Contacted Unresponsive | 2016 | 56 | ||||
| Contacted Unresponsive | 2017 | 31 | ||||
| Contacted Unresponsive | 2018 | 31 | ||||
| Contacted Unresponsive | 2019 | 22 | ||||
| Contacted Unresponsive | 2020 | 29 | ||||
| Contacted Unresponsive | 2021 | 30 | ||||
| Contacted Unresponsive | 2022 | 25 | ||||
| Unable to Contact | 2010 | 29 | ||||
| Unable to Contact | 2011 | 76 | ||||
| Unable to Contact | 2012 | 121 | ||||
| Unable to Contact | 2013 | 41 | ||||
| Unable to Contact | 2014 | 17 | ||||
| Unable to Contact | 2015 | 16 | ||||
| Unable to Contact | 2016 | 9 | ||||
| Unable to Contact | 2017 | 11 | ||||
| Unable to Contact | 2018 | 12 | ||||
| Unable to Contact | 2019 | 10 | ||||
| Unable to Contact | 2020 | 8 | ||||
| Unable to Contact | 2021 | 0 | ||||
| Unable to Contact | 2022 | 0 | ||||
| Unknown | 2010 | 313 | ||||
| Unknown | 2011 | 173 | ||||
| Unknown | 2012 | 147 | ||||
| Unknown | 2013 | 24 | ||||
| Unknown | 2014 | 0 | ||||
| Unknown | 2015 | 1 | ||||
| Unknown | 2016 | 0 | ||||
| Unknown | 2017 | 0 | ||||
| Unknown | 2018 | 0 | ||||
| Unknown | 2019 | 0 | ||||
| Unknown | 2020 | 0 | ||||
| Unknown | 2021 | 0 | ||||
| Unknown | 2022 | 0 | ||||
| Other | 2010 | 49 | ||||
| Other | 2011 | 78 | ||||
| Other | 2012 | 73 | ||||
| Other | 2013 | 124 | ||||
| Other | 2014 | 68 | ||||
| Other | 2015 | 44 | ||||
| Other | 2016 | 29 | ||||
| Other | 2017 | 38 | ||||
| Other | 2018 | 37 | ||||
| Other | 2019 | 54 | ||||
| Other | 2020 | 40 | ||||
| Other | 2021 | 32 | ||||
| Other | 2022 | 43 | ||||
Data Notes
New hearing screening objectives adopted in 2010 therefore trend data begins in 2010.Data Source
NBHS - HI*TRACK Hearing Screening Tracking and Data Management (C) HI*TRACK, Utah State UniversityNewborn hearing screening ENT-VSL-1.3: Infants with confirmed hearing loss enrolled for intervention services, Utah, 2010-2022
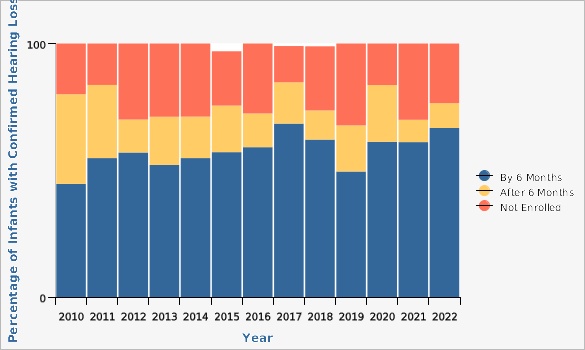
Infants with confirmed hearing loss should be enrolled in Early Intervention by 6 months of age to begin communication development as soon as possible.
| Timely Enrollment | Year | Percentage of Infants with Confirmed Hearing Loss | ||||
|---|---|---|---|---|---|---|
Record Count: 39 | ||||||
| By 6 Months | 2010 | 44.6% | ||||
| By 6 Months | 2011 | 54.8% | ||||
| By 6 Months | 2012 | 57.0% | ||||
| By 6 Months | 2013 | 52.1% | ||||
| By 6 Months | 2014 | 54.8% | ||||
| By 6 Months | 2015 | 57.1% | ||||
| By 6 Months | 2016 | 59.1% | ||||
| By 6 Months | 2017 | 68.4% | ||||
| By 6 Months | 2018 | 62.1% | ||||
| By 6 Months | 2019 | 49.5% | ||||
| By 6 Months | 2020 | 61.2% | ||||
| By 6 Months | 2021 | 61.1% | ||||
| By 6 Months | 2022 | 66.7% | ||||
| After 6 Months | 2010 | 35.4% | ||||
| After 6 Months | 2011 | 28.8% | ||||
| After 6 Months | 2012 | 13.0% | ||||
| After 6 Months | 2013 | 19.0% | ||||
| After 6 Months | 2014 | 16.4% | ||||
| After 6 Months | 2015 | 18.4% | ||||
| After 6 Months | 2016 | 13.3% | ||||
| After 6 Months | 2017 | 16.3% | ||||
| After 6 Months | 2018 | 11.5% | ||||
| After 6 Months | 2019 | 18.2% | ||||
| After 6 Months | 2020 | 22.4% | ||||
| After 6 Months | 2021 | 8.8% | ||||
| After 6 Months | 2022 | 9.8% | ||||
| Not Enrolled | 2010 | 20.0% | ||||
| Not Enrolled | 2011 | 16.4% | ||||
| Not Enrolled | 2012 | 30.0% | ||||
| Not Enrolled | 2013 | 28.9% | ||||
| Not Enrolled | 2014 | 28.8% | ||||
| Not Enrolled | 2015 | 21.4% | ||||
| Not Enrolled | 2016 | 27.6% | ||||
| Not Enrolled | 2017 | 14.3% | ||||
| Not Enrolled | 2018 | 25.3% | ||||
| Not Enrolled | 2019 | 32.3% | ||||
| Not Enrolled | 2020 | 16.4% | ||||
| Not Enrolled | 2021 | 30.1% | ||||
| Not Enrolled | 2022 | 23.5% | ||||
Data Notes
Infants not enrolled in Early Intervention may have opted-out when contacted by program staff for services or have been lost to follow-up. '''Over 98% of all children with confirmed hearing loss are referred to early intervention.''' Reasons for no EI enrollment are shown in [[a href="indicator/view/NewHearScr.EnrReas.html" ENT-VSL-1.3 (Part 2)]]. Lost to follow-up for Early Intervention has decreased since 2010: *2010: 10.8% *2011: 12.5% *2012: 19.0% *2013: 4.1% *2014: 8.7% *2015: 7.1%/3.1% removing "parent contacted unresponsive" *2016: 3.8% *2017: 1.0% *2018: 4.6% *2019: 6.5%/5.4% removing "parent contacted unresponsive" *2020: 1.5%/0.7% removing "parent contacted unresponsive" *2021: 6.2%/4.4% removing "parent contacted unresponsive" *2022: 2.0%/1.0% removing "parent contacted unresponsive" [[br]] [[br]] For 2015 (3), 2017 (1), and 2018 (1) there were children receiving only monitoring services so 100% of children are not accounted for in the graphs.Data Source
NBHS - HI*TRACK Hearing Screening Tracking and Data Management (C) HI*TRACK, Utah State UniversityNewborn hearing screening ENT-VSL-1.3 (Part 2): Reasons for no early intervention enrollment, Utah, 2013-2022
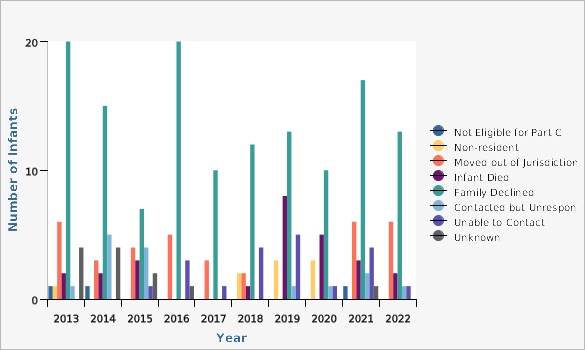
Documented reasons for not being enrolled in EI services include: not eligible for Part C, non-resident, moved out of jurisdiction, infant died, family declined, contacted but unresponsive, unable to contact, and unknown. Not included on this graph are "other" (2018=1, 2020=1) which are adoptions out of state and 2022 = 1 diagnosis changed to normal.
Utah EHDI has been actively working with the Utah School for the Deaf and Blind Parent Infant Program, as well as Baby Watch Early Intervention to determine reasons families decline Early Intervention services. This will guide future quality improvement initiatives.
| Reasons for No Enrollment | Year | Number of Infants | ||||
|---|---|---|---|---|---|---|
Record Count: 79 | ||||||
| Not Eligible for Part C | 2013 | 1 | ||||
| Not Eligible for Part C | 2014 | 1 | ||||
| Not Eligible for Part C | 2015 | 0 | ||||
| Not Eligible for Part C | 2016 | 0 | ||||
| Not Eligible for Part C | 2017 | 0 | ||||
| Not Eligible for Part C | 2018 | 0 | ||||
| Not Eligible for Part C | 2019 | 0 | ||||
| Not Eligible for Part C | 2020 | 0 | ||||
| Not Eligible for Part C | 2021 | 1 | ||||
| Not Eligible for Part C | 2022 | 0 | ||||
| Non-resident | 2013 | 1 | ||||
| Non-resident | 2014 | 0 | ||||
| Non-resident | 2015 | 0 | ||||
| Non-resident | 2016 | 0 | ||||
| Non-resident | 2017 | 0 | ||||
| Non-resident | 2018 | 2 | ||||
| Non-resident | 2019 | 3 | ||||
| Non-resident | 2020 | 3 | ||||
| Non-resident | 2021 | 0 | ||||
| Non-resident | 2022 | 0 | ||||
| Moved out of Jurisdiction | 2013 | 6 | ||||
| Moved out of Jurisdiction | 2014 | 3 | ||||
| Moved out of Jurisdiction | 2015 | 4 | ||||
| Moved out of Jurisdiction | 2016 | 5 | ||||
| Moved out of Jurisdiction | 2017 | 3 | ||||
| Moved out of Jurisdiction | 2018 | 2 | ||||
| Moved out of Jurisdiction | 2019 | 0 | ||||
| Moved out of Jurisdiction | 2020 | 0 | ||||
| Moved out of Jurisdiction | 2021 | 6 | ||||
| Moved out of Jurisdiction | 2022 | 6 | ||||
| Infant Died | 2013 | 2 | ||||
| Infant Died | 2014 | 2 | ||||
| Infant Died | 2015 | 3 | ||||
| Infant Died | 2016 | 0 | ||||
| Infant Died | 2017 | 0 | ||||
| Infant Died | 2018 | 1 | ||||
| Infant Died | 2019 | 8 | ||||
| Infant Died | 2020 | 5 | ||||
| Infant Died | 2021 | 3 | ||||
| Infant Died | 2022 | 2 | ||||
| Family Declined | 2013 | 20 | ||||
| Family Declined | 2014 | 15 | ||||
| Family Declined | 2015 | 7 | ||||
| Family Declined | 2016 | 20 | ||||
| Family Declined | 2017 | 10 | ||||
| Family Declined | 2018 | 12 | ||||
| Family Declined | 2019 | 13 | ||||
| Family Declined | 2020 | 10 | ||||
| Family Declined | 2021 | 17 | ||||
| Family Declined | 2022 | 13 | ||||
| Contacted but Unresponsive | 2013 | 1 | ||||
| Contacted but Unresponsive | 2014 | 5 | ||||
| Contacted but Unresponsive | 2015 | 4 | ||||
| Contacted but Unresponsive | 2016 | 0 | ||||
| Contacted but Unresponsive | 2017 | 0 | ||||
| Contacted but Unresponsive | 2018 | 0 | ||||
| Contacted but Unresponsive | 2019 | 1 | ||||
| Contacted but Unresponsive | 2020 | 1 | ||||
| Contacted but Unresponsive | 2021 | 2 | ||||
| Contacted but Unresponsive | 2022 | 1 | ||||
| Unable to Contact | 2013 | 0 | ||||
| Unable to Contact | 2014 | 0 | ||||
| Unable to Contact | 2015 | 1 | ||||
| Unable to Contact | 2016 | 3 | ||||
| Unable to Contact | 2017 | 1 | ||||
| Unable to Contact | 2018 | 4 | ||||
| Unable to Contact | 2019 | 5 | ||||
| Unable to Contact | 2020 | 1 | ||||
| Unable to Contact | 2021 | 4 | ||||
| Unable to Contact | 2022 | 1 | ||||
| Unknown | 2013 | 4 | ||||
| Unknown | 2014 | 4 | ||||
| Unknown | 2015 | 2 | ||||
| Unknown | 2016 | 1 | ||||
| Unknown | 2017 | 0 | ||||
| Unknown | 2018 | 0 | ||||
| Unknown | 2019 | 0 | ||||
| Unknown | 2020 | 0 | ||||
| Unknown | 2021 | 1 | ||||
Data Notes
Reasons for no Early Intervention enrollment were not collected on the CDC HSFS prior to 2013.Data Source
NBHS - HI*TRACK Hearing Screening Tracking and Data Management (C) HI*TRACK, Utah State UniversityNewborn hearing screening: Number of children with diagnosed hearing loss by birth year, Utah, 2010-2022
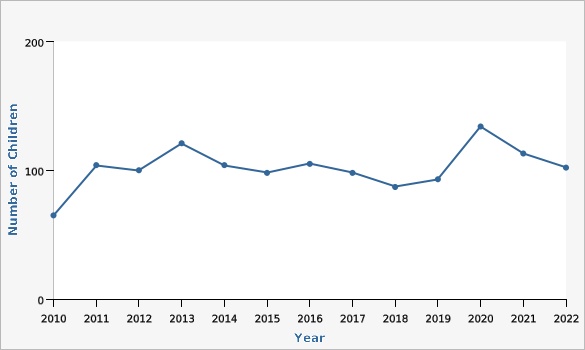
| Year | Number of Children | Note | ||||
|---|---|---|---|---|---|---|
Record Count: 13 | ||||||
| 2010 | 65 | * | ||||
| 2011 | 104 | |||||
| 2012 | 100 | |||||
| 2013 | 121 | * | ||||
| 2014 | 104 | |||||
| 2015 | 98 | |||||
| 2016 | 105 | |||||
| 2017 | 98 | |||||
| 2018 | 87 | |||||
| 2019 | 93 | |||||
| 2020 | 134 | |||||
| 2021 | 113 | |||||
| 2022 | 102 | |||||
Data Notes
*For 2010 data, HiTrack calculations for hearing loss were deemed to be inaccurate, under-representing the true number of children with hearing loss. *For 2013 data, calculations for hearing loss were deemed to be inaccurate, over-representing the true number of children with hearing loss due to many "undetermined" losses being counted as a permanent hearing loss. Incidence of permanent congenital hearing loss in Utah generally remains at 2 per thousand births.Data Source
NBHS - HI*TRACK Hearing Screening Tracking and Data Management (C) HI*TRACK, Utah State UniversityReferences and Community Resources
For an extensive list of Newborn Hearing Screening related links, please see the Utah Medical Home Portal website at [http://www.medicalhomeportal.org/newborn/hearing-loss-and-deafness]. National and local links are also available at [http://www.cdc.gov/ncbddd/hearingloss/index.html] and [http://infanthearing.org]. Regional resources for hearing screening and diagnostic services for newborn and infants can be found by visiting: [https://arcg.is/n4HmC] or by contacting the Utah EHDI Program at 801-273-6600 or ehdi@utah.gov.More Resources and Links
Evidence-based community health improvement ideas and interventions may be found at the following sites:- Centers for Disease Control and Prevention (CDC) WONDER Database, a system for disseminating public health data and information.
- United States Census Bureau data dashboard.
- Utah healthy Places Index, evidence-based and peer-reviewed tool, supports efforts to prioritize equitable community investments, develop critical programs and policies across the state, and much more.
- County Health Rankings
- Kaiser Family Foundation's StateHealthFacts.org
- Medical literature can be queried at PubMed library.
Page Content Updated On 02/06/2024,
Published on 03/07/2024